| Review Article Online Publishing Date: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Sudan J Paed. 2023; 23(2): 126-144 SUDANESE JOURNAL OF PAEDIATRICS 2023; Vol 23, Issue No. 2 REVIEW ARTICLE Determinants of cerebral palsy in children: systematic reviewKaleab Tesfaye Tegegne (1)Department of Public Health, College of Health Science, Debark University, Debark, Ethiopia Correspondence to: Kaleab Tesfaye Tegegne Department of Public Health, College of Health Science, Debark University, Debark, Ethiopia. Email: kaleabtesfaye35 [at] gmail.com Received: 09 December, 2022 | Accepted: 26 March 2023 How to cite this article: Tegegne KT. Determinants of cerebral palsy in children: systematic review. Sudan J Paediatr. 2023;23(2):126–144. https://doi.org/10.24911/SJP.106-1670589241 © 2023 SUDANESE JOURNAL OF PAEDIATRICS
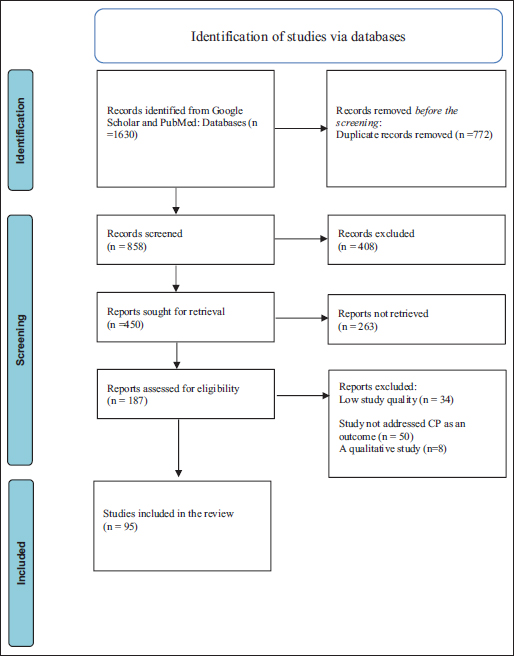
ABSTRACTCerebral palsy (CP) is a group of disorders of movement and postural control caused by a nonprogressive defect or lesion of the developing brain. Several prepregnancy risk factors have been described including maternal age, parity and maternal diseases including epilepsy, diabetes and thyroid disease. There are few in-depth studies on the causes of CP. In the present systematic review, databases searched were Google Scholar and PubMed to identify data on determinants of CP in the world. Studies were included if they specifically mentioned CP as an outcome, the study objective is to identify factors associated with CP in children and all quantitative observational studies. JBI Critical Appraisal Tools were used to assess the methodological quality of a study. Papers that meet the inclusion criteria were rigorously appraised by two critical appraisers. 40 consistent determinants of CP in children from 95 research articles that meet inclusion criteria are included in the review. The majority of studies (24 articles) showed that premature babies and low weight were determinants of CP in children, whereas 15 studies showed that low Apgar scores were determinants of CP in children. The commonest determinants of CP in children are premature babies and low weight, low Apgar scores, intrauterine infection, congenital brain malformations, thyroid disease, premature rupture of membrane (PROM) and placental abruption. Preventing preterm delivery, low birth weight and intrauterine infection as well as immediate neonatal resuscitation for newborns with low Apgar scores may help to prevent CP in children. KEYWORDS:Cerebral palsy; Determinants. INTRODUCTIONCerebral palsy (CP) is a group of disorders of movement and postural control caused by a nonprogressive defect or lesion of the developing brain [1]. According to population-based research conducted worldwide, the prevalence estimates for CP range from 1.5 to more than 4 per 1,000 live births [2–6]. In general, there are 2 cases of CP per 1,000 live births [7–9]. Chronic neurological conditions like CP place a heavy cost on the National Health System since they have a negative psychological and social impact on families. Medical and rehabilitation teams must work together to manage the treatment and rehabilitation of CP [10,11]. Prenatal, perinatal and neonatal risk factors are connected to CP. Perinatal asphyxia only accounts for less than 10% to 20% of instances of CP, with premature birth acknowledged as the primary risk factor [12–16]. Prematurity is one of the main CP risk factors [17,18]. Maternal age, parity and maternal illnesses such as epilepsy, diabetes and thyroid disease have all been listed as prepregnancy risk factors [19,20]. Risk factors that appear early or late in pregnancy include assisted reproduction, male gender, congenital malformations, multiple pregnancies and intrauterine growth restriction [21,22]. Fetal distress, premature rupture of the membrane, precipitous labor and jaundice are the key risk factors for CP [23]. In contrast, in a different study, the predictors were male gender, higher birth order, vaginal operations, central nervous system (CNS) illnesses in infants, unknown maternal education status and history of newborn hospital admissions [24]. Instrumental deliveries are risk factors for CP [25] and according to studies from Nigeria [26], Uganda [27] and Botswana [28], CP is linked to a history of CNS illness. Two studies found that CP risk factors were preterm and birth weight less than 1.5 kg [29,30]. Maternal anemia, maternal hypertension, pre-eclampsia, antepartum hemorrhage, eclampsia and multiple pregnancies are antenatal risk factors for CP [31]. Other African research has also implicated postnatal causes such as perinatal hypoxia, bilirubin encephalopathy, intracranial infections, ischemic stroke and congenital brain deformities as causal factors [32–34]. A Tanzanian study found that CP is mostly associated with prenatal issues [35]. A Ghanaian study also revealed that the most significant and curable risk factor for the onset of CP was severe neonatal hyperbilirubinemia [36]. Since CP is a chronic condition, it is essential to research and examine its causes, risk factors and interventional treatments to properly understand and manage the condition [37]. There are few in-depth studies on the causes of CP. A thorough discussion of risk factors linked to CP is provided in this systematic review. This systematic review identified CP risk factors that can be avoided, which lowers the prevalence of the condition. In this review, I have so tried to pinpoint the causes of CP in children. For the creation of preventive measures and treatments, a deeper comprehension of the CP etiology is required. The purpose of this review was to determine the factors that influence CP in children around the world. This systematic review identified consistent determinants of CP in children in two or more studies and this will help to develop a standard questionnaire as well as to construct a conceptual framework on determinants of CP in children. MethodsTo gather information on the global drivers of CP, I carried out a systematic evaluation of the literature that was available. Any study’s abstract from anywhere in the world was evaluated for inclusion. Criteria for inclusion were when the purpose of the study is to discover factors linked with CP in children, the study addressed CP as an outcome and all quantitative observational studies. The preferred reporting items for the systematic review and meta-analysis (PRISMA) 2020 checklist were followed (http://www.prisma-statement.org/). Search strategyTo locate pertinent English-language publications, various search techniques were used. I searched the databases of Google Scholar and PubMed using the terms ‘CP’, ‘determinants’, ‘risk factors’, and ‘CP’. I searched the World Health Organisation and international disability organisations’ websites for additional references that the previous search had overlooked. After screening the abstracts of any papers found using this search approach for relevance, the full texts of all pertinent articles were downloaded. A snowballing search was conducted after references from each pertinent article were checked for other pertinent articles. 95 research publications were included in the final review. Studies quality assessment toolJBI Critical Appraisal Tools available from (https://synthesismanual.jbi.global) for analytic crossectional study, case-control study and cohort study depending on study design used by researchers that meet the inclusion criteria were used to assess the methodological quality of a study and to determine the extent to which a study has addressed the possibility of bias in its design, conduct and analysis. All of the items in the checklist are rated based on the author’s subjective judgment given responses to the items rated as yes or no. Two reviewers independently evaluated the articles using the JBI critical appraisal checklist and the PRISMA checklist to determine whether they should be included in the review. All papers that meet the inclusion criteria were rigorously appraised by two critical appraisers. RESULTS95 research publications on determinants of CP in the world meet inclusion criteria and are included in the review [23–31,38–123]. A summary of CP risk factors in the included studies is presented in Table 1. The risk factors of CP are included in the identified list if the factors are associated with CP in two or more studies. I have identified 40 consistent risk factors of CP in children from 95 research articles that meet inclusion criteria and are included in the review. Factors seen in three categories:
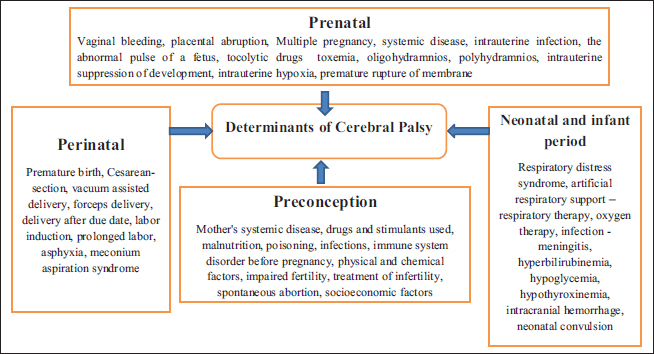
Prenatal risk factors associated with CP are urinary tract infection at pregnancy, transvaginal bleeding, perinatal hypoxia and prematurely, while postnatal risk factors are jaundice and convulsive syndrome [46]. Figure 1 shows the List of determinants of CP into four categories: Prenatal, perinatal, preconception and neonatal and infant period. Prematurity, low birth weight, twins or greater multiple births and prenatal infection are the main risk factors for CP (51). There were identified intrapartum-related, neonatal respiratory depression, neonatal encephalopathy and infections among the prenatal and perinatal determinants (neonatal sepsis, pneumonia, CNS infection, such as meningitis and encephalitis). There have been reports of postneonatal causes such as trauma, pneumonia and sepsis. Low socioeconomic status has also been linked to a higher chance of developing CP [49]. Congenital brain abnormalities, particularly defects of cortical development, are the primary causes of CP. More children with these problems can be diagnosed thanks to modern imaging techniques [56–58]. CP and congenital abnormalities are closely related [19,38,39,73,74]. In addition, there are more defects outside of the CNS in children with congenital brain deformities [122]. Other recognised prenatal causes of CP include maternal illnesses during the first and second trimesters of pregnancy (rubella, cytomegalovirus and toxoplasmosis) and vascular events seen by brain imaging (middle cerebral artery occlusion). Among the less frequent causes of CP are metabolic conditions, prenatal exposure to chemicals and uncommon genetic diseases. Neonatal encephalopathy is a clinically recognised syndrome that affects the neurological development of the term infant in the first few days of life. It is characterised by difficulties with breathing induction and maintenance, depression of tone and reflexes, subnormal levels of consciousness and frequent seizures [123]. Children with CP who have a history of neonatal encephalopathy are more likely than children without such a history to exhibit intrapartum hypoxia symptoms, such as meconium staining of the amniotic fluid, as well as a more severe form of the condition [68]. Using a grading system of 0 to III, a systematic investigation found a stronger correlation between CP and Sarnat Grade III encephalopathy than Sarnat Grade II encephalopathy [95]. CP may be caused by neonatal issues such as severe hypoglycemia, untreated jaundice and severe neonatal infection. Surgical procedures for congenital abnormalities and cerebrovascular accidents are two causes of postneonatally acquired CP [40]. Risk factors before pregnancyLong intermenstrual intervals, irregular menstruation and delayed menstruation are all related to an increased incidence of CP in mothers [39]. CP has also been linked to pregnancies that were particularly close together or far apart [39,103]. Low social class and CP are linked in children with normal birth weight, according to two studies [70,71]. In a study of preterm newborns, parity of three or more was a factor [57]. There is a connection between CP and past fetal fatalities, according to several researchers [73,81]. CP is linked to a number of maternal health issues. These include intellectual disability [73], seizures [73] and thyroid disease [19,73].
Figure 1. PRISMA 2020 flow diagram. Table 1. Summary of risk factors of CP on the included studies (N=95).
Figure 2. Determinants of cerebral palsy in children [107–112]. Paternal and sibling factorsSibling and paternal factors are rarely mentioned. More people with athetoid/dystonic CP have older fathers [102]. According to the Collaborative Perinatal Project of the National Institute of Neurological and Communicative Disorders and Stroke, motor deficiency in a sibling has been linked to CP [73]. DISCUSSIONRisk factors during pregnancyPregnancy-induced hypertension increases the risk of CP in children [59,79]. Pre-eclampsia is not associated with an increased risk of CP in preterm infants [51,86]. It has been suggested that preeclampsia may lead to a release of catecholamines in preterm infants, which accelerates fetal maturation [124]. Gestational diabetes increases the risk of CP in children [59,60]. Maternal trauma in pregnancy has been implicated as a possible cause of CP [87]. The rate of CP was increased in children whose mothers received thyroid hormone or estrogen in pregnancy [38] and with maternal thyroid abnormalities [19,82]. Two variants have been found that put heterozygous carriers at risk for venous thrombosis. One is the most frequent cause of familial thrombosis and is a mutation that is specific to the Factor V gene (Factor V Leiden mutation, VL). The prothrombin gene is the second. Caucasian women have a carrier frequency of 4.8%, compared to 5.5% in Caucasian men [125]. Current research in this area was sparked by a report of three infants with hemiplegic CP who were heterozygous for the Factor V Leiden mutation [126]. It was hypothesised that neonatal stroke or placental thrombosis may have occurred in the three cases documented and caused hemiplegia. Inflammatory mediators and indicators of autoimmune and coagulation disorders seem to be linked to CP [127]. Multiple pregnancies are linked to preterm labor, inadequate intrauterine growth, birth abnormalities and intrapartum problems in children [67,42,68]. Multiple pregnancies are also linked to CP in children [41,66,67]. However, the increased risk of prematurity and low birth weight in twins does not fully account for the increased risk of CP [128]. The loss of one twin during a monochorionic twin pregnancy is acknowledged as a significant risk factor for the co-twin who survives developing CP. The neurological growth of the surviving twin may be hampered during gestation if one twin passes away [135]. The main risk factor for the onset of CP appeared to be a lack of appropriate prenatal care. Infections during pregnancy were identified as significant risk factors. [130]. Some risk factors have repeatedly been observed to be related to CP, i.e., intrauterine viral infections (e.g., rubella and cytomegalovirus) [84,120–121], iodine deficiency [134], exposure to methyl mercury during pregnancy [82,111] and in Popayán, the main risk factor was maternal urinary tract infection [57]. Moreover, in another study, the most significant risk factors for the formation of CP were: untreated maternal anemia and the age of the mother over 30 years [58]. According to one study, term newborns with any disease during pregnancy, such as maternal hypertension, were more likely to have CP [60]. According to the gestational age group and clinical CP subtype, CP causes can differ to some extent. While spastic diplegia (legs affected more than arms) is the most common form of spastic involvement in preterm and very preterm newborns, hemiparetic (1-sided) and quadriparetic (4-limb) CP are the most common clinical subtypes in term and near-term infants. A perinatal stroke is a cerebrovascular accident that happens 28 days after birth while the baby is still a fetus or a newborn [93]. Compared to childhood or any other phase up to late middle age, the perinatal period has a significantly higher rate of stroke [59]. Newborns who are abnormally little or huge are more likely to get perinatal stroke than babies who are close to the average weight for the given dates [132]. Perinatal stroke has been linked to primiparity and a history of poor fertility and its treatment [78]. Perinatal stroke can cause CP in children. The risk of CP is higher in twins than in singletons and it is even higher in triplets. According to the available data, twin pregnancies and high-order multiple births’ propensity for early delivery and infant deaths account for the majority of factors that influence the risk of CP in multiple gestations. The highest incidence of CP was found among twins who survived whose co-twin was stillborn (4.5%), died soon after delivery (6.3%), or had CP (11.8%) in research that covered more than a million births [67]. Populations with high rates of consanguinity have documented familial aggregation of CP, and a national Swedish database found that families had an elevated chance of developing CP [112]. Preterm birth, placental abruption, preeclampsia and chorioamnionitis are a few maternal and pregnancy diseases that are risk factors for CP and have a genetic component. Many of the thrombophilias that cause prenatal strokes have hereditary roots. CP risk has been associated with genetic variations of apolipoprotein E [114] and a few inflammatory cytokines [113]. Exploratory research reveals that CP risk is influenced by nitric oxide synthase polymorphisms. [133,134]. The findings of research to date are consistent with roles for inflammation, coagulation, blood flow regulation and vascular endothelium function in the placenta and brain in CP pathobiology. Long maternal menstrual intervals have been linked to CP risk in three sizable population-based studies [38,39,80]. Polycystic ovarian syndrome (PCOS) is a significant contributor to abnormal menstrual spacing and is linked to other risk factors for CP, including perinatal stroke, obesity, preeclampsia, a procoagulant and proinflammatory state, preterm birth and the need for special care for the newborn [135]. In term newborns, maternal thyroid illness has been linked to CP [38], a decline in IQ [136] and congenital deafness [137]. During the antenatal period, placental abnormalities [138], intrauterine infections (TORCH infections), genital tract infections [116] and the threat of abortion [115,116], are the factors associated with CP in children. Meta-analysis showed that maternal hypertension during pregnancy was a risk factor for CP in children [43]. Maternal diabetes mellitus (DM) and thyroid diseases were more significant factors for CP in preterm patients [40,44], and in another study same result was found that maternal conditions (DM, thyroid diseases and medications during pregnancy) are risk factors for CP [83,84]. Antenatal determinants of CP are maternal medications (antibiotics and anti-epileptics) during pregnancy [115] and pre-eclampsia, in low–middle-income settings [64,65]. The main prenatal factor associated with CP was advanced mother age [58,62,102]. Risk factors during laborProlapsed cord, substantial intrapartum hemorrhage, protracted or violent birth due to cephalopelvic disproportion or atypical presentation, a large infant with shoulder dystocia and maternal shock from a variety of causes are major factors prone to induce perinatal asphyxia. [39]. The longer second stage of labor has also been linked to CP [81], emergency cesarean section [79], premature separation of the placenta [38] and abnormal fetal position [39]. When taking these elements into account, it is crucial to keep in mind that the event itself might not be the causal factor; instead, the event might just be linked to one or more actual causal factors. Significant evidence has recently emerged that chorioamnionitis, in particular, intrauterine exposure to infection in the final stages of pregnancy and after labor, is a significant risk factor for CP, especially in term newborns [51,80,88,89]. Chorioamnionitis was discovered to be a risk factor for both CP and periventricular leucomalacia in a meta-analysis of studies that examined the relationship between clinical and histological chorioamnionitis and CP or periventricular leukomalacia in both preterm and full-term infants [139]. It is necessary to learn more about how infections affect the prenatal period. Other associations with CP include prolonged rupture of the membranes in infants of all gestations [38] and preterm babies [51], the presence of meconium-stained fluid [84,90] and tight nuchal cord [127]. It has been suggested that magnesium sulfate, given for severe pre-eclampsia, is a protective factor in the development of CP in preterm infants [140,141]. CP risk increases with decreasing birth weight [39,51,54,55]. Both the gestational age at delivery and intrauterine growth affect birth weight. The length of gestation is the biggest predictor of CP, and the risk of the condition rises with advancing age at delivery [40]. Poor intrauterine growth also increases the risk of CP [94,95], particularly in moderately preterm [40]. It is not a major risk factor in very preterm infants [51,78]. There may be a connection between the rising number of low birth-weight babies with CP and their survival and future brain damage from birth defects such as intraventricular hemorrhage. Alternately, these children may have already been harmed before birth, and their preterm birth may have resulted from the same circumstances that affected them. Low placental weight [39] and low Apgar scores are strongly associated with CP [95]. Children with scores of 0–3 at five minutes had an 81-fold increased risk of CP [96]. Prematurity, low birth weight and asphyxia were selected risk factors related to the development of CP [56]. Delivery in a nonhospital setting appeared to be the major factor contributing to the development of CP. Important risk factors identified were home delivery and consanguinity [130]. Some risk factors have repeatedly been observed to be related to CP, i.e., low gestational age [52,53], low Apgar scores [94], preterm delivery and asphyxia [57]. Thus, the most significant risk factors for the formation of CP were tight entanglement of the umbilical cord and fetal hypoxia [58]. Maternal risk factors for CP include maternal infection, placental insufficiency and instrumental delivery. Perinatal factors include low birth weight [59]. One study showed that perinatal asphyxia, childbirth weight and delayed crying were independent factors associated with CP in term newborns [60]. Causal factors for spastic diplegia include evidence of intrauterine infection and PROM [41]. In a population-based study in northern California, evidence of maternal infection or fever during the admission for delivery was associated with the risk of CP in infants of normal birth weight, and with admission to a neonatal intensive care unit, neonatal seizures and meconium aspiration [120]. Chorioamnionitis and perhaps other infections seem to be a common antecedent to encephalopathy in the neonate and to later CP [145]. Repeated observations documented that intrauterine exposure to indicators of inflammation is linked with CP risk and that this is a common cause of low Apgar scores, other signs of neonatal depression, and CP risk [143]. Spontaneous abortion, abruptio placenta, prelabour rupture of membranes and prematurity were associated with a higher risk of CP. Preterm labor, Cesarean section, prematurity, asphyxia and low birth weight (<2500 g) were associated with an increased risk of CP [42]. During the intranatal period, uterine rupture increases the risk of CP in children [138]. The perinatal risk factors such as preterm, low birth weight and birth asphyxia, had a significant association with the development of CP [61]. Early membrane rupture, early delivery and emergency cesarean sections were all linked to an increased risk of CP in infants, according to a meta-analysis [43]. In preterm patients, persistent membrane rupture and maternal hemorrhage were the more important risk factors for CP [40,44]. Another study also found an association between CP and emergency CS [110]. Determinants of CP are PROM of long duration [45], antepartum fever [119], vaginal bleeding [85] and low birthweight (LBW) in low–middle-income settings [64,67]. Perinatal asphyxia was implicated as a cause of CP [64,65,91,92]. The main perinatal factors associated with CP were low Apgar scores, low birth weight and reduced gestational age [62]. Risk factors in the newborn periodNeonatal seizures [39,81], sepsis [19] and respiratory disease are associated with CP [81]. Reported risk factors in the preterm infant include patent ductus arteriosus, hypotension, blood transfusion, prolonged ventilation, pneumothorax, sepsis, hyponatremia, total parenteral nutrition, seizures and parenchymal damage with appreciable ventricular dilatation detected by cerebral ultrasound [97]. Neonatal seizures, in particular, are strongly associated with the risk of CP [39,97]. Gender and epilepsy were selected risk factors related to the development of CP [57]. Respiratory distress syndrome, prolonged ventilation, septicemia, meningitis, hyperbilirubinemia, neonatal seizures and severe cranial ultrasound abnormality were associated with an increased risk of CP in the neonatal period. In the postnatal period, the influence of indirect bilirubin on subcortical structures [116,121,144], hemolytic disease of newborns [121,144], septic conditions [98] and neonatal seizures had a significant association with the development of CP [61]. It is considered that the presence and severity of hypoxic-ischemic encephalopathy during the neonatal period is the strongest predictor of CP [32]. Kernicterus continues to be a significant problem in developing countries despite progress in the management of hyperbilirubinemia. In a clinic-based review in Nigeria, it was found that hyperbilirubinemia was the most common cause of CP [32]. This result is similar to another study [101]. Sepsis has been proven to increase the risk of developing CP, especially in preterm [99]. The antenatal risk factor of CP is CNS malformation [85]. In settings with few resources, there is a higher risk of newborn encephalopathy, according to studies from Nepal and Zimbabwe [47,146]; this may in turn increase the risk of developing CP. Increased levels of kernicterus been seen in research from West Africa [100] and outcome studies in Zimbabwe have revealed that 20% of newborns with severe jaundice dev have elop CP or motor impairment later in life [47]. The higher rates of jaundice reported are probably caused by untreated neonatal sepsis, G6PD deficiency, ABO and rhesus incompatibility, as well as by the delayed diagnosis and treatment of jaundice [147]. Malformation and small for gestational age births are still strongly linked to CP in children delivered moderately or late preterm [63]. Role of brain imagingEvidence on the timing of bad occurrences can be obtained via brain imaging, particularly magnetic resonance imaging (MRI). For instance, periventricular leukomalacia develops between the 28th and 34th week of pregnancy, and term infants with perinatal asphyxia have cortical and subcortical gliosis and atrophy in the parasagittal watershed areas. Cortical dysplasias also begin early in pregnancy, between the 12th and 20th week [148]. Despite being a major predictor of CP in preterm infants, periventricular leukomalacia is frequently seen in term infants, indicating that the detrimental event happened long before birth. Periventricular leukomalacia-causing factors may shed light on CP’s potential causes. [90,149]. According to studies, CP is linked to even the mother’s sociodemographic traits and reproductive history [150,151]. Prevention of CPWithin six hours of birth, therapeutic hypothermia is applied to prevent ischemia damage by stifling inflammatory cascades and apoptotic cellular processes. According to estimates, this treatment prevents the onset of CP symptoms in 1 in 8 newborns who receive it [152,153]. A substance being tested as a preventative measure is caffeine. The results of the caffeine for apnea of prematurity experiment show that caffeine lowers the incidence of CP in newborns with very low birth weight [152,154]. Early (8 days) postnatal steroid therapy is related to an increase in CP numbers despite the pulmonary advantages of prenatal betamethasone administration in preterm infants. The year 2010 saw recommendations from the American Academy of Pediatrics to reduce the use of postnatal corticosteroids [150,152,155,156]. Preterm newborns’ neuroprotection depends on the prenatal administration of magnesium sulfate. Through the reduction of pro-inflammatory cytokines, magnesium sulfate lowers the effects of inflammation. For mothers who are obese, the outcomes differ. It is prudent to note that there is disagreement on the application’s outcomes [152,157]. Infants with prenatal, perinatal and postnatal risk factors should have their motor development matched to their chronological age, with any residual primitive reflexes and delays in voluntary motor control being key diagnostic indicators. However, it is challenging to make a conclusive diagnosis before the age of two given that spasticity is not fully developed before 6 months, athetoid movements are not noticeable until the age of two, and persistent Babinsky reflexes are not noteworthy [158–160]. Therefore, without delay, every suspected baby should be enrolled in a rehabilitation program. The neurological examination will be supported by an MRI and laboratory testing, which will hasten the diagnosing procedure. Differential diagnosis is essential in this area as it is in every other area. After metabolic, hereditary and progressive neurological diseases have been ruled out, the conclusion is still possible. The European Database Group (SCPE) has determined that five is the ideal age to confirm a diagnosis based on the information above [161]. Further research into the involvement of infection in the prenatal period, studies into the impact of coagulation and inflammatory variables, and the use of advanced brain imaging are anticipated to yield more knowledge regarding the causes of CP. Current studies on the factors contributing to CP will be a crucial starting point for creating prevention methods. I would like to advocate addressing CP’s preventable causes, as doing so can lead to improved practice. CONCLUSIONThe commonest determinants of CP in children are premature babies and low weight, low Apgar scores, intrauterine infection, congenital brain malformations, premature rupture of the membranes and placental abruption. Preventing preterm delivery, low birth weight and intrauterine infection as well as immediate neonatal resuscitation for newborns with low Apgar scores may help to prevent CP in children. ACKNOWLEDGMENTThe author would like to thank Eleni Tesfaye Tegegne and Mekibib Kassa Tessema from the University of Gondar both of them worked as critical appraisers and Debark University, College of Health Science, for assisting me in doing this systematic review. CONFLICT OF INTERESTThere are no conflicts of interest stated by the author. FUNDINGThere was no financing available for this review. ETHICAL APPROVALEthics approval and consent to participate are not applicable. REFERENCES
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| How to Cite this Article |
| Pubmed Style Kaleab Tesfaye Tegegne. Determinants of cerebral palsy in children: systematic review. Sudan J Paed. 2023; 23(2): 126-144. doi:10.24911/SJP.106-1670589241 Web Style Kaleab Tesfaye Tegegne. Determinants of cerebral palsy in children: systematic review. https://sudanjp.com//?mno=93371 [Access: April 29, 2024]. doi:10.24911/SJP.106-1670589241 AMA (American Medical Association) Style Kaleab Tesfaye Tegegne. Determinants of cerebral palsy in children: systematic review. Sudan J Paed. 2023; 23(2): 126-144. doi:10.24911/SJP.106-1670589241 Vancouver/ICMJE Style Kaleab Tesfaye Tegegne. Determinants of cerebral palsy in children: systematic review. Sudan J Paed. (2023), [cited April 29, 2024]; 23(2): 126-144. doi:10.24911/SJP.106-1670589241 Harvard Style Kaleab Tesfaye Tegegne (2023) Determinants of cerebral palsy in children: systematic review. Sudan J Paed, 23 (2), 126-144. doi:10.24911/SJP.106-1670589241 Turabian Style Kaleab Tesfaye Tegegne. 2023. Determinants of cerebral palsy in children: systematic review. Sudanese Journal of Paediatrics, 23 (2), 126-144. doi:10.24911/SJP.106-1670589241 Chicago Style Kaleab Tesfaye Tegegne. "Determinants of cerebral palsy in children: systematic review." Sudanese Journal of Paediatrics 23 (2023), 126-144. doi:10.24911/SJP.106-1670589241 MLA (The Modern Language Association) Style Kaleab Tesfaye Tegegne. "Determinants of cerebral palsy in children: systematic review." Sudanese Journal of Paediatrics 23.2 (2023), 126-144. Print. doi:10.24911/SJP.106-1670589241 APA (American Psychological Association) Style Kaleab Tesfaye Tegegne (2023) Determinants of cerebral palsy in children: systematic review. Sudanese Journal of Paediatrics, 23 (2), 126-144. doi:10.24911/SJP.106-1670589241 |
Nagwa Salih, Ishag Eisa, Daresalam Ishag, Intisar Ibrahim, Sulafa Ali
Sudan J Paed. 2018; 18(1): 24-27
» Abstract » doi: 10.24911/SJP.2018.1.4
Siba Prosad Paul, Emily Natasha Kirkham, Katherine Amy Hawton, Paul Anthony Mannix
Sudan J Paed. 2018; 18(2): 5-14
» Abstract » doi: 10.24911/SJP.106-1519511375
Inaam Noureldyme Mohammed, Soad Abdalaziz Suliman, Maha A Elseed, Ahlam Abdalrhman Hamed, Mohamed Osman Babiker, Shaimaa Osman Taha
Sudan J Paed. 2018; 18(1): 48-56
» Abstract » doi: 10.24911/SJP.2018.1.7
Adnan Mahmmood Usmani; Sultan Ayoub Meo
Sudan J Paed. 2011; 11(1): 6-7
» Abstract
Mustafa Abdalla M. Salih, Mohammed Osman Swar
Sudan J Paed. 2018; 18(1): 2-5
» Abstract » doi: 10.24911/SJP.2018.1.1
Amir Babiker, Afnan Alawi, Mohsen Al Atawi, Ibrahim Al Alwan
Sudan J Paed. 2020; 20(1): 13-19
» Abstract » doi: 10.24911/SJP.106-1587138942
Hafsa Raheel, Shabana Tharkar
Sudan J Paed. 2018; 18(1): 28-38
» Abstract » doi: 10.24911/SJP.2018.1.5
Anita Mehta, Arvind Kumar Rathi, Komal Prasad Kushwaha, Abhishek Singh
Sudan J Paed. 2018; 18(1): 39-47
» Abstract » doi: 10.24911/SJP.2018.1.6
Majid Alfadhel, Amir Babiker
Sudan J Paed. 2018; 18(1): 10-23
» Abstract » doi: 10.24911/SJP.2018.1.3
Bashir Abdrhman Bashir, Suhair Abdrahim Othman
Sudan J Paed. 2019; 19(2): 81-83
» Abstract » doi: 10.24911/SJP.106-1566075225
Amir Babiker, Mohammed Al Dubayee
Sudan J Paed. 2017; 17(2): 11-20
» Abstract » doi: 10.24911/SJP.2017.2.12
Cited : 8 times [Click to see citing articles]
Mustafa Abdalla M Salih; Satti Abdelrahim Satti
Sudan J Paed. 2011; 11(2): 4-5
» Abstract
Cited : 4 times [Click to see citing articles]
Hasan Awadalla Hashim, Eltigani Mohamed Ahmed Ali
Sudan J Paed. 2017; 17(2): 35-41
» Abstract » doi: 10.24911/SJP.2017.2.4
Cited : 4 times [Click to see citing articles]
Amir Babiker, Afnan Alawi, Mohsen Al Atawi, Ibrahim Al Alwan
Sudan J Paed. 2020; 20(1): 13-19
» Abstract » doi: 10.24911/SJP.106-1587138942
Cited : 4 times [Click to see citing articles]
Mutasim I. Khalil, Mustafa A. Salih, Ali A. Mustafa
Sudan J Paed. 2020; 20(1): 10-12
» Abstract » doi: 10.24911/SJP.1061585398078
Cited : 4 times [Click to see citing articles]