| Case Report Online Published: 26 Dec 2023 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Sudan J Paed. 2023; 23(2): 243-247 SUDANESE JOURNAL OF PAEDIATRICS 2023; Vol 23, Issue No. 2 CASE REPORT Passive transfer of COVID-19 immunoglobulin via breast milk post COVID-19 vaccination of lactating mother: case report and review of the literatureSandeep Jhajra (1), Sarita Kumari (2), Chhavi Sauparna (1), Sanjay Kumar Tanti (1)(1) Department of Paediatrics, Tata Main Hospital, Jamshedpur, India (2) Department of Obstetrics and Gynaecology, Tata Main Hospital, Jamshedpur, India Correspondence to: Sandeep Jhajra Department of Paediatrics, Tata Main Hospital, Jamshedpur, India. Email: drsandeepjhajra [at] gmail.com Received: 25 September 2022 | Accepted: 17 November 2022 How to cite this article: Jhajra S, Kumari S, Sauparna C, Tanti SK. Passive transfer of COVID-19 immunoglobulin via breast milk post COVID-19 vaccination of lactating mother: case report and review of the literature. Sudan J Paediatr. 2023;23(2):243–247. https://doi.org/10.24911/SJP.106-1664086286 © 2023 SUDANESE JOURNAL OF PAEDIATRICS
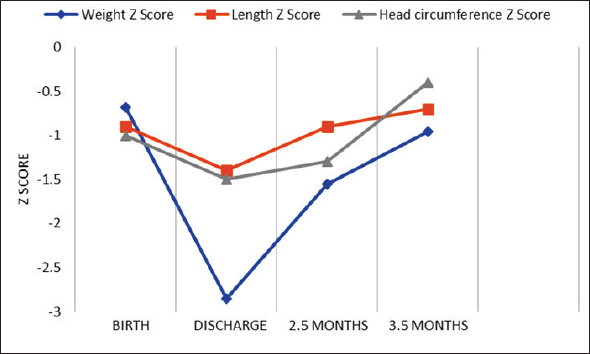
ABSTRACTInfant response against infections depends largely on active and passive transfer of immunity through breast milk. There is plenty of data showing transplacental transfer of anti-severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) antibodies to the foetus and the presence of neutralising Ig-A and Ig-G anti-SARS-CoV-2 antibodies in the breast milk of mothers post COVID-19 vaccination. There is a paucity of research regarding the impact of COVID-19 vaccination of lactating mothers on the immune response in infant blood. The index case was delivered at 35 weeks of gestation with features of hydrops fetalis. The COVID-19 rapid antigen test and COVID-19 reverse transcription-polymerase chain reaction test were negative for the mother and neonate. The baby was investigated for sepsis, underwent double volume exchange transfusion, and was discharged on exclusive breastfeeding. SARS-CoV-2 antibody titres were tested in blood and breast milk samples 4 weeks after first and second dose of the COVID-19 vaccination of the mother. Growth, neurodevelopment and haematological parameters were monitored over time. A robust immune response was reported in the blood of infants post COVID-19 vaccination of the mother with the potential to confer passive immunity to the baby and without any serious side effects in the mother-infant dyad. Keywords:Anti-SARS-CoV-2 IgG antibody; Breast feeding; COVID-19 vaccination. INTRODUCTIONThe severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) spread all over the world in the later half of 2019 and the World Health Organisation [1] declared it a pandemic on 11th March 2020. The development of a vaccination programme over a period of just 1 year against this deadly disease during recent times has been the perfect example of the strength of modern science. As of date 15th August 2022, a total of 2,085,387,344 doses of COVID-19 vaccine have been administered in India [2]. Initially, pregnant women and lactating mothers were not included in the vaccination drive due to a lack of safety data from the clinical trials [3]. After recommendations from many international and national bodies Government of India released a circular for the administration of the COVID-19 vaccine in pregnant and lactating mothers [4–7]. There is plenty of data showing the transplacental transfer of anti-SARS-CoV-2 antibodies to the foetus and the presence of neutralising Ig-A and Ig-G anti-SARS-CoV-2 antibodies in the breast milk of the mother post COVID-19 vaccination [8–12]. There is a paucity of research regarding the impact of COVID-19 vaccination of lactating mothers on immune response in infant blood. A single-centre study from the United States of America showed that vaccination during lactation fails to generate an immune response in infant blood despite the presence of SARS-CoV-2 antibody in maternal breast milk [8]. CASE REPORTThe index case was born to a 32-year-old fourth gravida Rh-ve mother at 35 weeks of gestation by lower segment Caesarean section (LSCS) in view of features of hydrops fetalis in the antenatal scan. Mother had no history of gestational diabetes mellitus, hypothyroidism, or hypertensive disorder of pregnancy. At the time of admission, she tested negative for COVID-19 infection by the reverse transcription-polymerase chain reaction (RT-PCR) screening test. The baby cried soon after birth with a birth weight of 2.25 kg. The baby had hepatosplenomegaly, ascites and severe respiratory distress. The baby was intubated and shifted to the neonatal intensive care unit. Mechanical ventilation and double surface intensive phototherapy were initiated. Surfactant was given within 2 hours of life and exchange transfusion was done in view of cord bilirubin of 7.43 mg/dl. An ascitic tap was done. Echocardiography showed normal structure and function of the heart (70% ejection fraction) with normal coronary arteries. An electrocardiogram revealed sinus rhythm. Chip-based RT-PCR test of baby for SARS-CoV-2 was negative at the time of admission. The sepsis screen came negative and gradually baby was weaned off to room air. Phototherapy was continued till day 6 of life. Laboratory parameters of the index case are shown in Table 1. Outcome and follow upThe baby remained hemodynamically stable throughout his stay and was discharged from the hospital on breastfeeds with advice for regular follow up in the high-risk clinic. Anthropometric parameters were monitored on follow up and Z scores were calculated (Figure 1). Table 1. Laboratory parameters of the neonate.
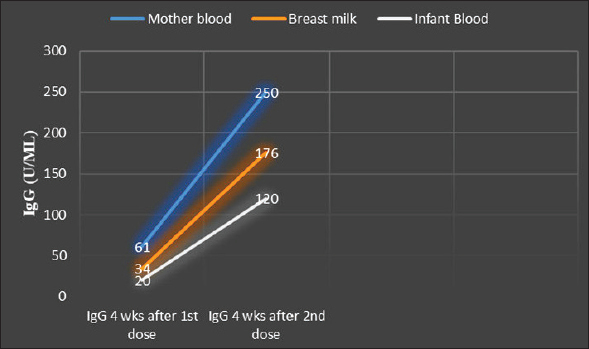
CSF, cerebrospinal fluid; Hb, haemoglobin; RT-PCR, reverse transcription polymerase chain reaction; SGOT, serum glutamic-oxaloacetic transaminase; SGPT, serum glutamic-pyruvic transaminase; TLC, total leukocyte count. Mother received the Covishield vaccine first dose at 4 weeks and second dose at 14 weeks after her delivery. Fever, chills and body aches were experienced by the mother after the first dose and the baby remained asymptomatic. IgG SARS-CoV-2 antibody titres were tested simultaneously in the blood of the mother and infant and breast milk, 4 weeks after first and second dose of COVID-19 vaccination of the mother (Figure 2). Anti-SARS-CoV-2 IgG levels were significantly elevated in the mother-infant dyad after the second dose of the COVID-19 vaccine. DISCUSSIONOur knowledge of immune response in infants post COVID-19 vaccination and COVID-19 infection of mothers is increasing rapidly by various studies across the globe. Multiple studies have shown transplacental transfer of COVID-19 antibodies in-utero to the foetus with persistence up to 6–8 months in infants [9,13,14]. Results of various trials showing the presence of IgG and IgA immunoglobulins against SARS-CoV-2 in breast milk post COVID-19 vaccination of breast-feeding mothers [11,12,15]. Young et al. [12] showed IgA predominance post COVID-19 infection and IgG dominant response post vaccination in the breast milk of lactating mothers [12]. The effect of stomach acidity on gastric IgG levels is lower in preterm neonates as compared to term infants. However, with increasing postmenstrual age gastric stability of IgG decreases [16]. Neonatal fragment crystallisable receptor in the intestine helps in bidirectional transcytosis of IgG in the gastrointestinal tract of infants [17]. In a cohort of eight infants of COVID-19 vaccinated mothers, Golan et al. [8] showed the failure of the generation of immune response in the blood of infants. In contrast, maternal vaccination seems to induce a robust immune response in our case. Index case has undergone exchange transfusion in view of features of hydrops fetalis and both mother and neonate tested negative for COVID-19. Transcytosis of IgG present in breast milk across intestinal epithelium seems to be the only explanation for detectable immune response in infant blood post maternal COVID-19 vaccination. There are a few limitations of our study. First, functional assays were not performed and second, breast milk of the lactating mother was not tested for SARS-CoV-2 IgG antibodies past 180 days after vaccination, which would have provided intriguing correlates. This is the first time when anti SARS-CoV-2 IgG antibodies are seen in the blood of infants of lactating mothers post COVID-19 vaccination. Our findings will motivate lactating mothers to get vaccinated and to continue breastfeeding post vaccination.
Figure 1. Growth of index cases over the period.
Figure 2. Anti-SARS-CoV-2 IgG levels of mother and infant. CONCLUSIONIn summary, we report a robust immune response in the blood of infants post COVID-19 vaccination of the mother with the potential to confer passive immunity to the baby and without any serious side effects in the mother-infant dyad. There are no long-term sequelae on growth and neurodevelopment. Adequately powered studies will help in the confirmation of our findings. CONFLICT OF INTERESTSThe authors declare no conflict of interest. FUNDINGNone. CONSENT FOR PUBLICATIONConsent from parents was taken. ETHICAL APPROVALSigned informed consent for participation and publication of medical details was obtained from the parents. Confidentiality of patient data were ensured at all stages. The authors declare that ethics committee approval was not required for this case report. REFERENCES
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| How to Cite this Article |
| Pubmed Style Jhajra S, Kumari S, Sauparna C, Tanti SK. Passive transfer of Covid-19 immunoglobulin via breast milk post Covid vaccination of lactating mother: case report and review of literature. Sudan J Paed. 2023; 23(2): 243-247. doi:10.24911/SJP.106-1664086286 Web Style Jhajra S, Kumari S, Sauparna C, Tanti SK. Passive transfer of Covid-19 immunoglobulin via breast milk post Covid vaccination of lactating mother: case report and review of literature. https://sudanjp.com//?mno=117336 [Access: February 05, 2026]. doi:10.24911/SJP.106-1664086286 AMA (American Medical Association) Style Jhajra S, Kumari S, Sauparna C, Tanti SK. Passive transfer of Covid-19 immunoglobulin via breast milk post Covid vaccination of lactating mother: case report and review of literature. Sudan J Paed. 2023; 23(2): 243-247. doi:10.24911/SJP.106-1664086286 Vancouver/ICMJE Style Jhajra S, Kumari S, Sauparna C, Tanti SK. Passive transfer of Covid-19 immunoglobulin via breast milk post Covid vaccination of lactating mother: case report and review of literature. Sudan J Paed. (2023), [cited February 05, 2026]; 23(2): 243-247. doi:10.24911/SJP.106-1664086286 Harvard Style Jhajra, S., Kumari, . S., Sauparna, . C. & Tanti, . S. K. (2023) Passive transfer of Covid-19 immunoglobulin via breast milk post Covid vaccination of lactating mother: case report and review of literature. Sudan J Paed, 23 (2), 243-247. doi:10.24911/SJP.106-1664086286 Turabian Style Jhajra, Sandeep, Sarita Kumari, Chhavi Sauparna, and Sanjay Kumar Tanti. 2023. Passive transfer of Covid-19 immunoglobulin via breast milk post Covid vaccination of lactating mother: case report and review of literature. Sudanese Journal of Paediatrics, 23 (2), 243-247. doi:10.24911/SJP.106-1664086286 Chicago Style Jhajra, Sandeep, Sarita Kumari, Chhavi Sauparna, and Sanjay Kumar Tanti. "Passive transfer of Covid-19 immunoglobulin via breast milk post Covid vaccination of lactating mother: case report and review of literature." Sudanese Journal of Paediatrics 23 (2023), 243-247. doi:10.24911/SJP.106-1664086286 MLA (The Modern Language Association) Style Jhajra, Sandeep, Sarita Kumari, Chhavi Sauparna, and Sanjay Kumar Tanti. "Passive transfer of Covid-19 immunoglobulin via breast milk post Covid vaccination of lactating mother: case report and review of literature." Sudanese Journal of Paediatrics 23.2 (2023), 243-247. Print. doi:10.24911/SJP.106-1664086286 APA (American Psychological Association) Style Jhajra, S., Kumari, . S., Sauparna, . C. & Tanti, . S. K. (2023) Passive transfer of Covid-19 immunoglobulin via breast milk post Covid vaccination of lactating mother: case report and review of literature. Sudanese Journal of Paediatrics, 23 (2), 243-247. doi:10.24911/SJP.106-1664086286 |
Nagwa Salih, Ishag Eisa, Daresalam Ishag, Intisar Ibrahim, Sulafa Ali
Sudan J Paed. 2018; 18(1): 24-27
» Abstract » doi: 10.24911/SJP.2018.1.4
Siba Prosad Paul, Emily Natasha Kirkham, Katherine Amy Hawton, Paul Anthony Mannix
Sudan J Paed. 2018; 18(2): 5-14
» Abstract » doi: 10.24911/SJP.106-1519511375
Inaam Noureldyme Mohammed, Soad Abdalaziz Suliman, Maha A Elseed, Ahlam Abdalrhman Hamed, Mohamed Osman Babiker, Shaimaa Osman Taha
Sudan J Paed. 2018; 18(1): 48-56
» Abstract » doi: 10.24911/SJP.2018.1.7
Adnan Mahmmood Usmani; Sultan Ayoub Meo
Sudan J Paed. 2011; 11(1): 6-7
» Abstract
Mustafa Abdalla M. Salih, Mohammed Osman Swar
Sudan J Paed. 2018; 18(1): 2-5
» Abstract » doi: 10.24911/SJP.2018.1.1
Amir Babiker, Afnan Alawi, Mohsen Al Atawi, Ibrahim Al Alwan
Sudan J Paed. 2020; 20(1): 13-19
» Abstract » doi: 10.24911/SJP.106-1587138942
Bashir Abdrhman Bashir, Suhair Abdrahim Othman
Sudan J Paed. 2019; 19(2): 81-83
» Abstract » doi: 10.24911/SJP.106-1566075225
Anita Mehta, Arvind Kumar Rathi, Komal Prasad Kushwaha, Abhishek Singh
Sudan J Paed. 2018; 18(1): 39-47
» Abstract » doi: 10.24911/SJP.2018.1.6
Majid Alfadhel, Amir Babiker
Sudan J Paed. 2018; 18(1): 10-23
» Abstract » doi: 10.24911/SJP.2018.1.3
Amir Babiker, Mohammed Al Dubayee
Sudan J Paed. 2017; 17(2): 11-20
» Abstract » doi: 10.24911/SJP.2017.2.12