| Review Article Online Publishing Date: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Sudan J Paed. 2023; 23(2): 112-125 SUDANESE JOURNAL OF PAEDIATRICS 2023; Vol 23, Issue No. 2 CURRENT OPINION Paediatric career decision: a literature review of motivational factorsJubran Alqanatish (1,2,3), Abdulmajeed Alfadhel (1,2,3), Areej Albelali (1,2,3), Dhafer Alqahtani (4)(1) King Abdullah Specialized Children’s Hospital, King Abdulaziz Medical City, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia (2) King Abdullah International Medical Research Center, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia (3) King Saud Bin Abdulaziz University for Health Sciences, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia (4) Department of Cardiology, Prince Sultan Cardiac Center, Riyadh, Saudi Arabia Correspondence to: Jubran Alqanatish King Abdullah Specialized Children’s Hospital, King Abdulaziz Medical City, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia Email: qanatishj [at] mngha.med.sa.Authors Received: 30 September 2023 | Accepted: 14 November 2023 How to cite this article: Alqanatish J, Alfadhel A, Albelali A, Alqahtani D. Paediatric career decision: a literature review of motivational factors. Sudan J Paediatr. 2023;23(2):112–125. https://doi.org/10.24911/SJP.106-1696066895 © 2023 SUDANESE JOURNAL OF PAEDIATRICS
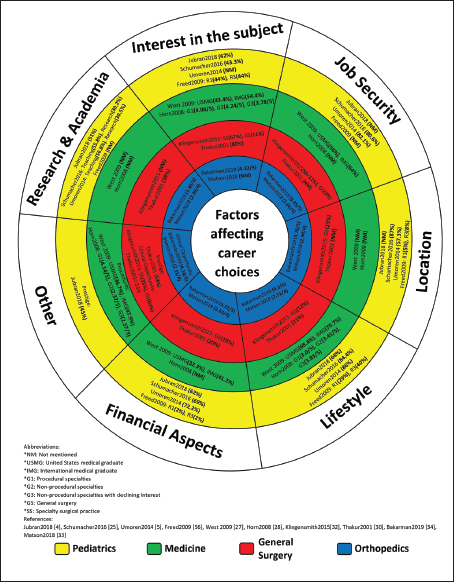
ABSTRACTUnless decision-makers for the future paediatric workforce are aware of different factors that influence the career choices of candidates, they may not be able to meet the needs of this major specialty. Paediatricians should be perceptive, effective communicators and endlessly patient with children. In this article, we conducted a thorough literature search to explore factors affecting career choices among undergraduate and postgraduate students who choose paediatrics or paediatric subspecialties. We assessed the similarities and differences in decision-making in paediatric, medicine, surgery and orthopaedic career contexts to help the candidates in ranking their career options. The authors found that both intrinsic and extrinsic factors shape the career choices of those seeking to work in paediatrics or paediatric subspecialties. A well-structured career development curriculum and clinical experience are considered the most important extrinsic factors, whereas personal characteristics of the candidate and career needs are considered the most important intrinsic factors. These factors may vary across specialties, and even between different subspecialties within the same major specialty. Some factors are considered very important, while others are deemed less so in comparison. The role of mentoring in career selection is crucial. It has been documented in a sizable body of literature that residents are inspired to pursue the careers of their mentors. Paediatrics is no exception. The decision to pursue a subspecialty training is complex and is affected by multiple factors. Those engaged in managing the workforce of the future in the field of paediatrics must familiarise themselves with the intrinsic and extrinsic factors that affect the candidates’ career choices. KEYWORDS:Paediatric workforce; Career decision-making; Mentorship; Extrinsic factors; Intrinsic factors. INTRODUCTIONMaking decisions concerning the paediatric workforce of the future is not possible without understanding how people who chose paediatrics as a career arrived at their final decision. Intrinsic and extrinsic factors shape career choices. Extrinsic factors include career development curriculums and clinical exposure or experience, whereas intrinsic factors mainly include career needs and personal characteristics of the candidate. As one’s career progresses, there will be a shift in influence from intrinsic to extrinsic factors [1,2]. Mentorships have a close link with career choices. Residents tend to have solid career plans for the future if they are mentored [3]. In an earlier survey of 282 paediatric residents, we found that 43% of the residents had received satisfactory counselling in the course of selecting their careers [4]. Paediatrics residents who were mentored by subspecialists were more likely to pursue careers in their mentors’ subspecialties after graduation, rather than careers in general paediatrics [5]. The timing of decisions pertaining to future careers tended to vary. In our above mentioned study of paediatric residents in Saudi Arabia, we found that over 60% had chosen their future subspecialties during residency [4]. Mahoney et al. [6] reported that doctors who were considering careers in specialties that have a shortage were encouraged to pursue careers in these specialties if they received early career counselling in medical school and immediately after graduation. This article presents a review of the literature on factors that affect career choices among undergraduate and postgraduate students who intend to pursue paediatrics or paediatric subspecialties. We also look at the differences and similarities between career choices trending toward paediatrics and other specialties. The main aim is to equip decision-makers for the future paediatric workforce (leaders responsible for clinical aspects and education in paediatrics) with a better understanding of the different factors that influence career choices. CHARACTERISTICS OF A PAEDIATRICIANCurrently, there are over 60 specialties available for medical graduates to choose from. Paediatric medicine is a highly satisfying career option, as taking care of children goes beyond providing individualised care. A candidate considering a career in paediatrics must be equipped with resources that can influence that choice and help them build a successful career [7]. Dealing with children is not easy. It is essential for a physician dealing with children to have the skills necessary to build rapport with babies, preschool, school and teenage children [8]. Sometimes, children may not pay attention and may squirm during a physical examination. Dealing with adolescents requires unique skills that can help build good relationships based on trust after obtaining information on their medical history. Therefore, it is very important for a paediatrician to be able to speak the adolescent’s language and to adapt their communication to gain their trust. Being patient is a key factor in enabling a paediatrician to deal with children wisely [9]. Parental understanding of child health issues is also crucial for childcare. This cannot happen without effective communication with the attending doctor, and thus, being an excellent communicator is a vital attribute for a paediatrician as well [10]. American Academy of Paediatrics states that effective communication and response to the demands of the child and family dynamics is the cornerstone of childcare [10,11]. Health determinants vary across communities and families. Paediatricians need to be aware of all issues that may affect a child’s development, growth and general well-being, such as educational, cultural, socioeconomic and racial factors. Paediatricians should always remember that families handle various challenges differently [9]. Consequently, being a paediatrician necessitates a unique combination of various distinctive skills. Paediatricians should be perceptive, effective communicators and endlessly patient with children. CURRICULUM OF CAREER DEVELOPMENTCareer development is best described as supporting a trainee in gaining new skills or in reshaping and cultivating their existing skills. It includes professional development and enhancement of job proficiency, interview skills, job-seeking skills and career planning activities. Cifra et al. [12] conducted a survey of 129 paediatric critical care fellows and junior faculty members in 2017 to understand the rubrics of an academic career development curriculum. They found that about 50% had an academic career development curriculum during their fellowship. As many as 43% of fellows identified the fellowship programme director as a competent mentor who helped them in their career development journey [12]. This finding was consistent with those of Rama et al. [13] who found that a well-structured career development curriculum can ease the transition into academic faculty positions for most paediatric fellowship graduates. There are well-established associations between career development support and career satisfaction and proficiency [13]. Career development support is given to academic-based clinicians as opposed to community-based (non-academic) clinicians. This is because fellowship programmes mainly operate in academic settings and do not necessarily address community needs. Career development curriculums have received more attention from those who are interested in academic and research careers as opposed to those who are interested in clinical track careers [12]. TIMING OF A PAEDIATRIC CAREER CHOICEKnowing when paediatric residents make their decisions about careers during the residency training programme is crucial for clarifying the distribution of physicians in subspecialties early enough, and is vital in any attempt to tackle the needs of children across the US [14]. This is true and known as physician manpower planning in any country. However, little is known about when paediatric residents make up their minds about their careers. Macy et al. [14] surveyed 7,580 paediatric residents during each year of their residency programmes between 2010 and 2014. The majority (4,963 respondents, 65.5%) intended to pursue fellowships after their residency programmes. Of these, 2,843 (57%) enrolled in paediatric subspecialty fellowship training programmes from 2013 to 2016. Most residents, that is, 1,944 (68%), indicated having plans to enter fellowship training programmes right from the first year of the residency programme. Male residents reported having plans to pursue fellowship programmes earlier than female residents. During the residency programme, it was most common for residents (27.6%) to select specific subspecialties in their second year. Approximately 20% of the residents changed their subspecialties during residency [14]. A study by Freed et al. [15] examined 2,300 paediatric residents and followed them between 2007 and 2009. In 2007, 69% (1,592*) of the residents decided on their future career directions and 708 (31%) were still unsure. In 2009, 504 out of 708 residents (71%) made their career choices during the residency programme. Most paediatric residents decided to pursue fellowships or careers in primary care before starting the residency course [15]. In our previous cross-sectional study of 282 residents across five main cities in Saudi Arabia for the academic year 2016–2017 [4], we found that 10% chose their future careers during medical school, 27% during their internship, and 63% during residency programme [4]. Exposure to paediatric subspecialties throughout medical school and the residency programme has an effective influence on career choices. Most residents have a clear career plan from the beginning of their residency training programmes. Early decision-making should be encouraged among paediatric residents so that decision-makers in the field can address the needs of children and shape the future paediatric workforce appropriately. THE ROLE OF MENTORSHIP IN CAREER DEVELOPMENTMentorships are key to successful career development, especially for young doctors in training [16]. Literature has reported that mentorship is associated with prosperous personal and career development, career selection and outstanding research skills [17–19]. The paucity of mentorship was found to be an obstacle to career development by 98% of the respondents in a study of 16 academic physicians [16]. A study by Umoren and Frintner [5] reported that 87% of paediatric residents had mentors during residency training programmes. Mentorships seem rare among internal medicine residents. A study by Ramanan et al. [3] surveyed internal medicine residents and reported that only 56% had mentors during their residency programmes. They found that most mentees found mentorship useful and beneficial. They also described that over two-thirds of the respondents had stated that mentorship had a significant impact on their professional development, while 57% reported that it had a valuable effect on their personal development [3]. Jubran et al. [4] reported that 43% of paediatric residents had received satisfactory counselling for their career choices. They found a substantial link between mentorship in residents and their likelihood of deciding their future subspecialties [4]. However, no studies have examined the negative impacts of mentorship on career choices. Not all mentoring relationships are successful, Ramanan et al. [3] found about 25% of the residents offered negative feedback on mentorship, saying that they felt uncomfortable talking about ‘important issues’, whereas 14% said that they felt like they were a burden on their mentors. In another study, 11 anaesthesiology residents and 12 faculty physicians were interviewed and it was found that different kinds of goal-setting activities and expectations of mentors and mentees led to negative mentoring relationships and resulted in inevitable disappointment and termination of the mentoring relationship [20]. The timing of mentorship was also found to be a significant influence on career choices, as discovered in a survey of 99 general surgery postgraduates [21]. McCord et al. [21] reported that participants who had found mentors before engaging in the residency programme were more likely to pursue non-academic careers, while most participants who chose academic routes were those who had found mentors during the residency programme. Residents tend to choose their areas of practice and subspecialties in the first 2 years of the residency programme; therefore, being mentored during these years is an advantage [21]. Although mentorship is important in career decisions and can affect subspecialty choices in paediatrics, there is no evidence of its impact on the type of practice selected, in comparison to other specialties [22]. The Accreditation Council for Graduate Medical Education (ACGME) programme requirements for graduate medical education comprise a section on paediatrics, with a specific focus on curriculum organisation and resident experiences. Understatement number IV.C.6.a).(1), states thus: ‘The individualized curriculum must be determined by the learning needs and career plans of each resident and must be developed through the guidance of a faculty mentor’ [23]. Established mentorship programmes have reported promising outcomes by nurturing residents’ skills in many areas such as research, clinical work and career development. After eliminating other confounding factors such as career choices at the beginning of the training programme and the individual residents’ traits, mentees with subspecialist mentors were found to be 70% more likely to subspecialise instead of opting for general practice, than when they were with a generalist mentor [5]. Umoren and Frintner [5] reported that 93% of the mentees in paediatric residency programmes had chosen the same specialties as their mentors. FACTORS THAT INFLUENCE SUBSPECIALTY CHOICE AFTER A RESIDENCY PROGRAMMEMedicine is divided into several specialties. Selecting a particular specialty for life is a hard task. When it comes to choosing a subspecialty, it can be even harder. Several factors affect a resident’s choice of specialty. Some are considered very important, and others, are less so. In addition, some factors predominate in one community due to their cultural background, that other communities do not take into account or consider less important, that is why some factors predominate in one country more than others. Harris et al. [24] conducted a survey of 238 paediatric residents and graduates from the Children’s Hospital of Philadelphia over a period of 12 years and found that almost all residents, especially women aged under 30 years, deemed lifestyle considerations as important. Jubran et al. [4] examined paediatric residents in Saudi Arabia and reported that gender did not affect lifestyle considerations among their respondents. This statement contradicts previous literature which found that females were more likely to consider lifestyle considerations and flexibility in working hours while choosing a subspecialty [22]. Interest in a specific disease or patient population and financial considerations were also found to be important for over half of the Saudi Arabian paediatric residents [4]. Other factors that are deemed important in choosing a subspecialty include technical/procedural skills, research opportunities, teaching/academic opportunities, job security, positive impact of role models, geographic location and intellectual stimulation [4,22,24]. Other factors such as personal preferences, job accomplishment and personal debt ranked lower [4,22]. In another study, 1,000 paediatric residents were surveyed to understand the relationship between residency programme size and career selection, and it concluded that the importance of certain factors such as teaching, research interest and specific patient populations increase as the programme size increases [25]. The impact of these factors can also be affected by the country in which the programme takes place. For example, a study in India by Sneha et al. [26] reported that the most common factor in selecting paediatrics as a career choice was interest in the subject, whereas Schumacher et al. [25] found that the geographical location of the future job was the most important factor in choosing paediatrics as a career in the US. Residents value factors differently while deciding between pursuing general paediatrics and a subspecialty. Those who seek to pursue general paediatrics consider lifestyle and personal or financial concerns; whereas, those who seek to pursue a subspecialist career are more likely to consider their interest in the disease and/or the specific patient population, technical and/or procedural skills and teaching and research opportunities over other factors [22,24]. A summary of factors affecting career choices in the field of paediatrics is provided in Table 1. Similarly, those pursuing internal medicine specialties treat lifestyle and family considerations as the most important factors in career selection. West et al. [30] conducted a cross-sectional survey of 14,890 internal medicine residency graduates on their career decisions and found that lifestyle was most often treated as important, whereas future income, technical skills and mentor specialty were deemed less important. Women tend to value lifestyle and long-term relationships with patients while choosing subspecialties, and do not focus much on future income [30]. Financial issues were mainly considered by residents who had debts totalling over $150,000 [30,31]. In a two-phase study by Horn et al. [31], 110 internal medicine residents were surveyed and found that men tended to select subspecialties involving procedural and/or technical skills, prestigious reputation and financial security. In selecting subspecialties with no procedural interventions, lifestyle and patient population were found to be the most common factors considered [31]. A study done in Canada showed that personal interest in the subject area was treated as the most important factor, followed by clinical rotation in specialty, mentor specialty and job security; the least important factors were lifestyle and financial issues, location and the resident’s own reasons [32]. A summary of factors affecting career choices in medicine is provided in Table 2. Surgical residents made their future career choices after considering multiple factors. Thakur et al. [33] reported that among surgical residents in the general surgery programme at the University of California, Los Angeles, 93% indicated interest in the field as one of their top three influences and 80% considered it as the main factor. Over half of the residents (53%) also stated that surgical field prestige was an important factor [33]. Mentor’s surgical skills, accomplishments and verbal recommendations on their subspecialties influenced 45% of the residents. The least important factors were income (20%), family priorities (13%), lifestyle (11%) and length of training (2%) [33]. Table 1. Factors affecting career choices in the field of paediatrics.
NM: not mentioned; R: resident. Incorvaia et al. [34] conducted a survey among randomly selected surgical residents from 40 different general surgery residency programmes across the United States. As many as 53% of the residents planned to pursue fellowships and they considered the potential of the specialty as the most important factor, whereas salary and the ability to repay debts were deemed least important in choosing their future careers [34]. Klingensmith et al. [35] conducted a survey of 3,354 surgery residency graduates from 2009 to 2013, and found that 26% were planning to pursue general surgery, and 74% intended to pursue specialty surgical practice [35]. Among the latter, 57% mentioned that personal interest was their major motivation, whereas 35% indicated that an interest in refining their skills and experience motivated them to pursue specialty training [35]. Among the former, 63% stated that diversity of procedures was a main influence in their decision to pursue general surgery, 56% indicated that a positive mentor played a major role in influencing their career decisions and 54% credited a wide range of practice areas as a key factor in their choice. The least significant aspects were family commitments (12%) and financial motivations (10%) [35]. A summary of factors affecting career choices in general surgery is provided in Table 3. Table 2. Factors affecting career choices in medicine.
G: group; IMG: international medical graduate; NM: not mentioned; USMG: United States medical graduate. In the orthopaedic surgery specialty, intellectual provocation and diversity of surgical procedures were found to be the main important factors that impact subspecialty selection in a survey conducted among 359 orthopaedic residents [36]. Bakarman et al. [37] studied 108 orthopaedic surgeons who were residents, fellows or consultants, in Saudi Arabia. Among the Saudi orthopaedic residents, the most essential factor in deciding on a subspecialty was the prognosis of the patient with a mean score of 4.41, followed by a personal interest in the specialty (4.32) and variability of cases (4.14); considering 5 as strongly agree and 1 as strongly disagree. [37]. A summary of factors affecting career choices in orthopaedics is provided in Table 4. Table 3. Factors affecting career choices in general surgery.
GS: general surgery; NM: not mentioned; SS: specialty surgical practice. Table 4. Factors affecting career choices in orthopaedics.
N: number; NM: not mentioned. The decision to pursue subspecialty training is complex and is affected by several factors that could be related to the training centre, the subspecialty or the residents themselves. Paediatrics has diverse subspecialties such as cardiology, critical care, neurology, rheumatology, genetics, hepatology, gastroenterology, haemato-oncology, neonatology, developmental paediatrics, nephrology, immunology and endocrinology [26]. Dattner and Ozuah [22] cross-sectionally surveyed 355 paediatric residents and found that 73% had made up their minds on their career intentions and 63% aimed at pursuing subspecialties. They also reported that men tended to subspecialise more frequently than women. Furthermore, there was no difference between the timing of career decisions and the likelihood of sub-specialisation [22]. In our study of residents in Saudi Arabia, we found that women were more likely to choose endocrinology and cardiology, whereas men were more inclined to select gastroenterology and paediatric emergency medicine [4]. In India, 89% of the women surveyed said that they considered marriage as a major factor that influenced their career choices, whereas 92% of the men surveyed considered it irrelevant [26]. Involving trainees in routine procedures performed as part of a subspecialty can increase their likelihood of pursuing a subspecialty [26]. Schumacher et al. [25] correlated residency programme size and career decisions and reported that many trainees in small residency programmes chose to subspecialise and a large number of residents in large programmes chose primary fields of care; this shows that career intentions do not always align with clinical rotations and experience. DIFFERENCES AND SIMILARITIES BETWEEN CAREERS IN PAEDIATRICS AND OTHER SPECIALTIESA medical graduate’s choice of specialty depends on certain individual preferences. Some are met during the residency training programme and others are shaped during the training phase. The literature has indicated that lifestyle and family considerations were the most significant factors that influenced paediatric residents’ career choices [4,22,24] and that these factors were considered more important by women than men [22,24]. We also found that more than half of the Saudi residents we studied identified financial concerns as an important factor motivating their career decisions [4]. The literature on internal medicine residents has shown that lifestyle considerations and financial security have a crucial impact on career choices and have a greater value for women than for men [30,31]. On the other hand, surgical residents reported that they were influenced more by their personal interests in particular specialties while pursuing their career choices [33–35]. Unlike in the case of internal medicine and paediatric residents, surgical residents were less affected by financial considerations while making their career choices [33–35]. This may be because of the prevailing perceptions among surgeons that there is not much of a variance in income among various surgical specialties [33]. The effect of mentorship on residents depends on the specialty. The mentorship was found to be beneficial and influential for surgical residents [21,31,33,35]. Thakur et al. [33] indicated that mentor supervision motivated 44% of the residents and 66% of the surgical residents they studied to pursue the same careers as their mentors. Paediatric residents were five times more likely to select their mentors’ subspecialties [5]. Mentorship had a minor impact on internal medicine residents and their career decisions [30,32]. Factors affecting career choices among paediatrics, medicine, general surgery and orthopaedic specialties are summarised in Figure 1. CAREERS IN ACADEMIC PAEDIATRICS AND CLINICAL RESEARCHThe literature reports that there are many barriers to research such as: ‘insufficient research training, lack of dedicated research time and deficiency in academic mentorship and role models’ [38]. Academic practitioners with a tendency to pursue a career in research are most likely to decide their career trajectories in the course of their residency training because they are provided with well-organised mentorship and goal-setting support [39]. Many clinicians face tremendous dissatisfaction when they aspire to be mentored to acquire research skills after working for a while in academic institutions [40]. We can thus conclude that timing is an important factor in learning and being mentored for those seeking careers in research. Therefore, it is recommended that research mentorships and support for career decisions be made available during the residency programme so that residents can pursue their career choices successfully. Ragsdale et al. [40] interviewed junior faculty and staff physicians engaged in hospital medicine and general paediatrics at a large academic institution and found that most physicians agreed that the lack of mentorships was a fundamental factor that motivated their decision not to pursue a research career.
Figure 1. Factors affecting career choices. Another study that examined factors that affect research and career choices surprisingly found that having research requirements in the residency stage did not inspire residents to pursue careers in research or academia [41]. This seems different from the findings in internal medicine residency programmes that nearly 30% of residents had stated that a research requirement had an impact on their career selection [42]. Stern et al. [43] conducted a survey among the participants in an emergency medicine residency and found that financial support and funding were linked to an increase in the probability of pursuing a career in research. Segal et al.’s [41] study contradicted this as he found that access to financial support did not influence career decisions. Administrative and individual factors also play a role in determining research career choices. Administrative factors include departmental interest and training, mentorship, financial support and availability of time for research. Individual factors include interest in research, multitasking skills, capacity to balance clinical and other work, reading, research skills and future career intentions [41]. Many physicians dedicate time and effort to research to get promoted academically since promotion has been greatly linked to a number of first-author peer-reviewed publications. Reid et al. [44] surveyed nearly 400 academic hospitalists, which correlated the number of publications with the academic positions they held. To clarify this further, after the same number of years of expertise in academic medicine, an assistant professor had published one or two first-author peer-review publications when compared to an associate professor who had a greater number of publications (four to six). Furthermore, an academic hospitalist who got promoted to the position of a professor had been working for 5 or more years with at least eight first-author peer-review publications [44]. Atasoylu et al. [45] surveyed Department of Medicine chairs across the US and Canada and concluded that teaching and clinical skills were primary elements for the promotion of clinician educators. PAEDIATRICIANS AS ADVOCATES FOR CHILDRENEvery child deserves a paediatrician who advocates in favour of their rights and responds to their needs. Advocacy addresses several issues ranging from the child’s well-being to community health needs [46]. From medical and legal points of view, children do not have the capacity to make decisions about their own health. All decisions pertaining to their health and well-being are made by their parents or guardians on their behalf. Unfortunately, parents or guardians may neglect or underestimate their children’s care needs. As many as 25.9% of children aged between 6 months and 4 years, 29.4% of children aged between 5 and 9 years and 20.6% of children aged between 10 and 15 years reported having experienced at least one form of neglect [47]. Therefore, an advocating paediatrician is crucial for promoting child health as they work toward the protection of children from neglectful and overprotective guardians. About 22% of the children in the United States live at or below the poverty line. In developing countries such as Sudan, Ahmed et al. [48], have reported that 41% and 63% urban and rural families live below the poverty line, respectively. As many as 52.4% of the children in India are below the poverty line [49]. This state will ultimately lead to a rising number of chronic diseases and morbidity, accidental injuries, malnourishment and limited access to healthcare [50,51]. Understanding how to advocate for children’s rights effectively is an important component in paediatric residency training as it can improve children’s health [46]. Nevertheless, despite many published articles emphasising the significance of advocacy for children’s rights, effective advocacy skills are sometimes omitted in paediatric training programmes [52–56]. The ACGME has required all paediatric residency training programmes to consider advocacy for children’s rights as a core element in their curriculums [23]. The Royal College of Physicians and Surgeons of Canada and the Canadian paediatric residency programmes have mandated the prioritisation of advocacy for children’s rights in the training area [57]. For this to happen, paediatric residency training programmes should emphasis advocacy for children’s rights. Advocacy skills can be acquired in a manner that is similar to how clinical decision-making skills are acquired, that is, through experience and problem-based learning [54]. While not all paediatric residents will be pulmonologists or nephrologists, every paediatrician has to be an advocate for children’s rights [46]. CONCLUSIONResidents value factors differently when choosing to pursue a career in general paediatrics or a subspecialty of paediatrics. Graduate residents in paediatrics and internal medicine consider lifestyle and future income as important factors in deciding their subspecialties. In contrast, it was found that over half of surgical residents consider personal interest as an important factor in determining their specialties. Orthopaedic residents select their subspecialties based on intellectual provocation and diversity in surgical procedures. The role of mentorships in shaping career decisions is crucial. It is clear that residents are inclined toward the careers of their mentors. Paediatrics is no exception to this. Overall, the decision to pursue a subspecialty is complex and is affected by multiple factors. Those engaged in managing the workforce of the future in the field of paediatrics must familiarise themselves with the intrinsic and extrinsic factors that affect their career choices. ACKNOWLEDGEMENTThe authors would like to thank Editage (www.editage.com) for English language editing. CONFLICT OF INTERESTThe authors declare no conflict of interest. FUNDINGNone. ETHICAL APPROVALNot applicable. REFERENCES
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| How to Cite this Article |
| Pubmed Style Alqanatish J, Alfadhel A, Albelali A, Alqahtani D. Pediatric career decision: A literature review of motivational factors. Sudan J Paed. 2023; 23(2): 112-125. doi:10.24911/SJP.106-1696066895 Web Style Alqanatish J, Alfadhel A, Albelali A, Alqahtani D. Pediatric career decision: A literature review of motivational factors. https://sudanjp.com//?mno=171476 [Access: April 27, 2024]. doi:10.24911/SJP.106-1696066895 AMA (American Medical Association) Style Alqanatish J, Alfadhel A, Albelali A, Alqahtani D. Pediatric career decision: A literature review of motivational factors. Sudan J Paed. 2023; 23(2): 112-125. doi:10.24911/SJP.106-1696066895 Vancouver/ICMJE Style Alqanatish J, Alfadhel A, Albelali A, Alqahtani D. Pediatric career decision: A literature review of motivational factors. Sudan J Paed. (2023), [cited April 27, 2024]; 23(2): 112-125. doi:10.24911/SJP.106-1696066895 Harvard Style Alqanatish, J., Alfadhel, . A., Albelali, . A. & Alqahtani, . D. (2023) Pediatric career decision: A literature review of motivational factors. Sudan J Paed, 23 (2), 112-125. doi:10.24911/SJP.106-1696066895 Turabian Style Alqanatish, Jubran, Abdulmajeed Alfadhel, Areej Albelali, and Dhafer Alqahtani. 2023. Pediatric career decision: A literature review of motivational factors. Sudanese Journal of Paediatrics, 23 (2), 112-125. doi:10.24911/SJP.106-1696066895 Chicago Style Alqanatish, Jubran, Abdulmajeed Alfadhel, Areej Albelali, and Dhafer Alqahtani. "Pediatric career decision: A literature review of motivational factors." Sudanese Journal of Paediatrics 23 (2023), 112-125. doi:10.24911/SJP.106-1696066895 MLA (The Modern Language Association) Style Alqanatish, Jubran, Abdulmajeed Alfadhel, Areej Albelali, and Dhafer Alqahtani. "Pediatric career decision: A literature review of motivational factors." Sudanese Journal of Paediatrics 23.2 (2023), 112-125. Print. doi:10.24911/SJP.106-1696066895 APA (American Psychological Association) Style Alqanatish, J., Alfadhel, . A., Albelali, . A. & Alqahtani, . D. (2023) Pediatric career decision: A literature review of motivational factors. Sudanese Journal of Paediatrics, 23 (2), 112-125. doi:10.24911/SJP.106-1696066895 |
Nagwa Salih, Ishag Eisa, Daresalam Ishag, Intisar Ibrahim, Sulafa Ali
Sudan J Paed. 2018; 18(1): 24-27
» Abstract » doi: 10.24911/SJP.2018.1.4
Siba Prosad Paul, Emily Natasha Kirkham, Katherine Amy Hawton, Paul Anthony Mannix
Sudan J Paed. 2018; 18(2): 5-14
» Abstract » doi: 10.24911/SJP.106-1519511375
Inaam Noureldyme Mohammed, Soad Abdalaziz Suliman, Maha A Elseed, Ahlam Abdalrhman Hamed, Mohamed Osman Babiker, Shaimaa Osman Taha
Sudan J Paed. 2018; 18(1): 48-56
» Abstract » doi: 10.24911/SJP.2018.1.7
Adnan Mahmmood Usmani; Sultan Ayoub Meo
Sudan J Paed. 2011; 11(1): 6-7
» Abstract
Mustafa Abdalla M. Salih, Mohammed Osman Swar
Sudan J Paed. 2018; 18(1): 2-5
» Abstract » doi: 10.24911/SJP.2018.1.1
Amir Babiker, Afnan Alawi, Mohsen Al Atawi, Ibrahim Al Alwan
Sudan J Paed. 2020; 20(1): 13-19
» Abstract » doi: 10.24911/SJP.106-1587138942
Hafsa Raheel, Shabana Tharkar
Sudan J Paed. 2018; 18(1): 28-38
» Abstract » doi: 10.24911/SJP.2018.1.5
Anita Mehta, Arvind Kumar Rathi, Komal Prasad Kushwaha, Abhishek Singh
Sudan J Paed. 2018; 18(1): 39-47
» Abstract » doi: 10.24911/SJP.2018.1.6
Majid Alfadhel, Amir Babiker
Sudan J Paed. 2018; 18(1): 10-23
» Abstract » doi: 10.24911/SJP.2018.1.3
Bashir Abdrhman Bashir, Suhair Abdrahim Othman
Sudan J Paed. 2019; 19(2): 81-83
» Abstract » doi: 10.24911/SJP.106-1566075225
Amir Babiker, Mohammed Al Dubayee
Sudan J Paed. 2017; 17(2): 11-20
» Abstract » doi: 10.24911/SJP.2017.2.12
Cited : 8 times [Click to see citing articles]
Mustafa Abdalla M Salih; Satti Abdelrahim Satti
Sudan J Paed. 2011; 11(2): 4-5
» Abstract
Cited : 4 times [Click to see citing articles]
Hasan Awadalla Hashim, Eltigani Mohamed Ahmed Ali
Sudan J Paed. 2017; 17(2): 35-41
» Abstract » doi: 10.24911/SJP.2017.2.4
Cited : 4 times [Click to see citing articles]
Amir Babiker, Afnan Alawi, Mohsen Al Atawi, Ibrahim Al Alwan
Sudan J Paed. 2020; 20(1): 13-19
» Abstract » doi: 10.24911/SJP.106-1587138942
Cited : 4 times [Click to see citing articles]
Mutasim I. Khalil, Mustafa A. Salih, Ali A. Mustafa
Sudan J Paed. 2020; 20(1): 10-12
» Abstract » doi: 10.24911/SJP.1061585398078
Cited : 4 times [Click to see citing articles]