| Review Article Online Published: 26 Dec 2023 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Sudan J Paed. 2023; 23(2): 224-233 SUDANESE JOURNAL OF PAEDIATRICS 2023; Vol 23, Issue No. 2 ORIGINAL ARTICLE Rhythm abnormalities among hospitalised children in Lagos: a case seriesBarakat A. Animasahun (1,2), Alaba B. Oladimeji (2), Moriam O. Lamina (2), Adaobi U. Solarin (1,2), Elizabeth A. Disu (1,2)(1) Department of Paediatrics and Child Health, Lagos State University College of Medicine, Ikeja, Nigeria (2) Department of Paediatrics, Lagos State University Teaching Hospital, Ikeja, Nigeria Correspondence to: Barakat A. Animasahun Department of Paediatrics and Child Health, Lagos State University College of Medicine, Ikeja, Nigeria. Email: deoladebo [at] yahoo.com Received: 27 July 2019 | Accepted: 17 November 2023 How to cite this article: Animasahun BA, Oladimeji AB, Lamina MO, Solarin AU, Disu EA. Rhythm abnormalities among hospitalised children in Lagos: a case series. Sudan J Paediatr. 2023;23(2):224–233. https://doi.org/10.24911/SJP.106-1564007487 © 2023 SUDANESE JOURNAL OF PAEDIATRICS
ABSTRACTArrhythmias refer to disturbances in heart rate or rhythm which leads to heart rates that are abnormally fast, slow or irregular. Rhythm abnormalities may be common among Nigerian children but there are only a few reports. The current write up is a clinical review of eight patients in various age groups including neonates, infants and older children. It is presented to highlight the different forms of arrhythmias that can occur in children, with varying underlying aetiology, thus, stressing the need for early recognition of arrhythmias in children, appropriate early intervention and challenges involved in their care. KeywordsRhythm abnormalities; Children; Arrhythmia; Lagos; Aetiology; Dysrhythmia. INTRODUCTIONArrhythmias refers to disturbances in heart rate or rhythm which leads to heart rates that are abnormally fast, slow or irregular [1]. Either slow or fast arrhythmias may lead to acutely decreased cardiac output and deterioration into a more dangerous arrhythmia such as ventricular fibrillation, or if unremitting may lead to cardiomyopathy [1]. They may also lead to syncope and sudden death [1]. Globally, primary clinically significant arrhythmias are much less common in children compared to adults [2]. In the United States, the overall incidence of paediatric arrhythmia is 55.1 per 100,000 paediatric emergency visits and the incidence of clinically significant arrhythmia is estimated at 22.5 per 100,000 paediatric patients [2,3]. A retrospective study from Australia also reported the incidence of arrhythmias amongst children less than 18 years admitted into an emergency unit at a tertiary hospital was 140 per 100,000 over a 6-year period [4]. A population-based study in England reported the incidence of arrhythmias in infants as 24.4 per 100,000 live births [5]. Arrhythmias may be transient or incessant, congenital or acquired. It may be caused by toxins or drugs [1]. They may be associated with particular forms of congenital heart disease (CHD) such as atrial septal defect or Ebstein anomaly. Arrhythmias may also be a complication of surgical repair of CHD such as tetralogy of Fallot. It may also complicate metabolic disorders such as hypokalaemia and hypocalcaemia. Arrhythmia can also be caused by endocrine abnormalities, genetic diseases and foetal inflammation from maternal connective tissue disorders [1]. There are two clinically significant mechanisms responsible for the formation of arrhythmias: an abnormal formation of the electric impulse (abnormal automaticity) or a change in conduction or re-entry [6]. Supraventricular tachycardia (SVT) is the most commonly reported arrhythmia in children [7–9]. The true incidence of SVT, as well as other rarer forms of arrhythmias such as atrioventricular block and ventricular tachycardia, in children, is unknown but has been estimated to be 1 in 250 to 1 in 1,000 children [10]. The clinical presentation of arrhythmias depends on the aetiology, underlying rhythm disorder and the age at presentation [11]. Neonates and infants tend to present with features of congestive cardiac failure while older children present with palpitation and syncope [11]. The treatment depends on the type and underlying aetiology. In Nigeria, there are few reports on the burden, spectrum and clinical features of paediatric arrhythmias among Nigerian children. For example, Sadoh et al. [12] reported the incidence of arrhythmia in a hospital-based study of children seen at an emergency department to be 1 in 265, while Animasahun et al. [13] reported only two cases of SVT over a 10-year period. Tabansi and Dibua [14] evaluated 1,002 secondary school students in Port-Harcourt for subclinical arrhythmia: 3.8% of the studied subjects had abnormal electrocardiogram (ECG) findings which included 12 persons with bundle branch block. The current retrospective review of eight children who were diagnosed and managed over a period of 5 years at three hospitals in Lagos seeks to add to the body of knowledge on the pattern and presentation of paediatric clinical arrhythmias. MATERIALS AND CASE REPORTSA summary of the eight cases described below is presented in Table 1. Case 1A 25-day-old female term neonate was admitted via the emergency room with a history of fast breathing noticed on the seventh day of life. There was no history of cough, easy fatigue during breastfeeding, diaphoresis or cyanosis. Her mother commenced antenatal care at 13 weeks gestation at a private hospital; she had no febrile illness in pregnancy and started routine haematinics in the first trimester and, in addition, herbal medication at the seventh month of gestation. There was no history of exposure to radiation, pregnancy-induced hypertension or gestational diabetes mellitus. She had three obstetrics ultrasound scans which all revealed foetal bradycardia. There was no history of prolonged rupture of membrane or prolonged labour. She was born at term to a 26-year-old primiparous woman. She cried well at birth and her birth weight was 2.3 kg. Direct breastfeeding was commenced on the third day of life. On examination, she was in respiratory distress, tachypnoeic and centrally cyanosed. Oxygen saturation was 44% in room air. The apex beat was at the fifth left intercostal space lateral to the midclavicular line. She was bradycardic with a heart rate of 52 beats per minute (bpm), the first and second heart sounds were heard on auscultation. Chest radiograph showed cardiomegaly. The electrocardiograph showed bradycardia and a second-degree heart block Mobitz type 2. Echocardiography revealed a complete atrioventricular septal defect, moderate-sized secundum atrial septal defect, interrupted inferior vena cava, total anomalous pulmonary venous connection and moderate to severe hypertension. Packed cell volume and serum electrolyte were normal. A diagnosis of complex cyanotic congenital heart defects with heart block was made. Parents were counselled to do Holter monitoring ECG and for surgical intervention. She was commenced on intravenous atropine. However, she died on the fifth day of admission. Table 1. Demographic, clinical, electro- and echocardiographic characteristics of eight children managed for arrhythmias in Lagos, Nigeria.
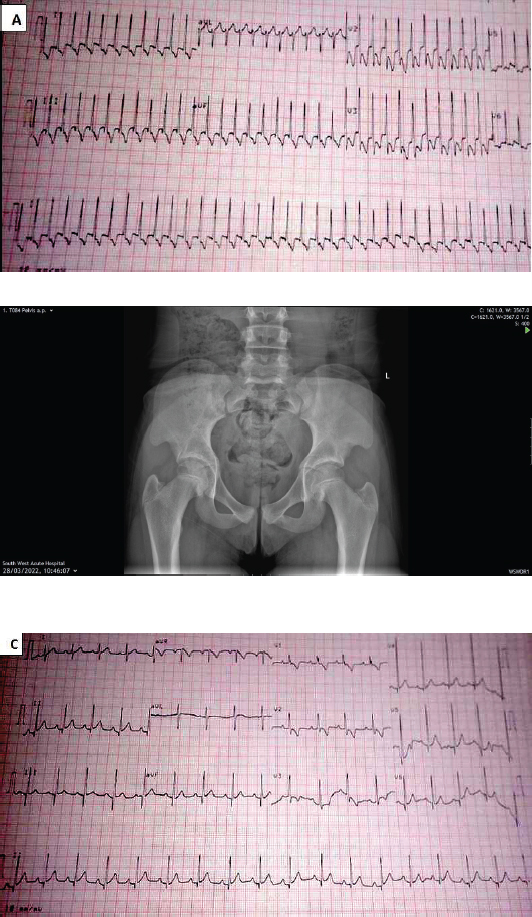
M: Male; AVSD: atrioventricular septal defect; MV: mitral valve; SVT: supraventricular tachycardia; F: female; ASD: atrial septal defect; AV; aortic valve; MR: mitral regurgitation; ECG: electrocardiogram; PAH: pulmonary artery hypertension; LV: left ventricle; PS: pulmonary stenosis; TAPVC: total anomalous pulmonary venous connection. Case 2A male, term neonate presented with fever on the 10th day of life at the outpatient clinic with no other symptoms. The pregnancy was uneventful. He was born at term via emergency caesarean section in a private hospital on account of foetal bradycardia. He cried well at birth, the birth weight was 3 kg and he was commenced on breastmilk. On examination at presentation, he was cyanosed but not dyspnoeic with oxygen saturation of 85% in room air. Cardiovascular examination revealed the apex beat at the fourth right intercostal space, the heart rate was 64 bpm which was irregularly irregular with a grade 3 pansystolic murmur. A diagnosis of a heart block secondary to a cyanotic CHD was made. Electrocardiography showed second-degree heart block Mobitz type 2. Echocardiography revealed a dextrocardia, total anomalous pulmonary venous connection, large secundum atrial septal defect, mild pulmonary stenosis and severe pulmonary hypertension. He was admitted, monitored and subsequently discharged when the fever resolved without any intervention. A Holter monitoring ECG was requested. Parents were counselled for urgent surgical intervention. He was however re-admitted 2 weeks after discharge, following aspiration of feeds while his mother was feeding. On examination, he was in respiratory distress, cyanosed with oxygen saturation of 58% in room air, the respiratory rate was 62 cycles per minute (cpm), the heart rate was 63 bpm and rhonchi were heard on auscultation. He was commenced on oxygen and nebulised with salbutamol. His clinical condition improved and he was subsequently discharged. He had a surgical intervention in India at the age of 6 months with a pacemaker insertion. Unfortunately, the pacemaker inserted could not be interrogated with the Medtronic pacemaker interrogator available in our centre necessitating its replacement with Medtronic in a private centre recently at the age of 3 years 4 months. The patient had a wound infection after the procedure and died 2 weeks after the surgery. Case 3A female newborn presented on the 12th day of life with a history of low-grade, continuous fever, fast breathing and abdominal distension noticed on the 9th day of life. The fast breathing progressively worsened but no history of cyanosis and cough. Abdominal distension was not associated with vomiting and constipation. Her mother administered an herbal concoction at the onset of the symptoms. The pregnancy was supervised by a traditional birth attendant. She took herbal concoction all through pregnancy. Delivery was via spontaneous vaginal delivery but there was a poor cry at birth. The birth weight was unknown but the weight at presentation was 1.58 kg. On examination, she was conscious, dyspnoeic and acyanosed with a respiratory rate of 68 cpm. The heart rate was 68 bpm, and no murmur was heard on auscultation. The abdomen was mildly distended with no organs palpable. A diagnosis of a small gestational-age baby with neonatal sepsis and possibly CHD was made. She was admitted and had investigations including complete blood count which showed leucocytosis with neutrophilia, and urgent electrocardiograph which showed bradycardia with a second-degree heart block Mobitz type 2. Echocardiography showed a common atrium, complete atrioventricular septal defect. She was commenced on antifailure drugs and her mother was counselled on the need for cardiac surgery. She was subsequently discharged but was lost to follow up in the clinic. Case 4A 3-month-old male presented with a history of low-grade intermittent fever and fast breathing of 1 day duration. Fast breathing progressively worsened and was not associated with cough, catarrh, cyanosis, excessive sweating or prolonged feeding time. He had episodes of inconsolable cries. On examination, he was irritable in respiratory distress, afebrile, not cyanosed and oxygen saturation in room air was 83%–91%. The heart rate was 150 bpm, and no murmur was heard. The respiratory rate was 52 cpm with vesicular breath sounds. A diagnosis of possibly acute bronchiolitis was made. He was admitted and commenced on intranasal oxygen. The chest radiograph was normal. He had hypokalaemia which was corrected. On further review, he was noticed to have desaturated despite being on 100% oxygen. He became lethargic, sweating profusely with his heart rate ranging between 295 and 300 bpm. An urgent electrocardiograph revealed SVT (Figure 1A) and echocardiography showed a structurally normal heart. There was no response to vagal manoeuvre. He was transferred to the intensive care unit. Systolic blood pressure recordings were in the hypotensive range between 60 and 65 mmHg while the diastolic was not recordable. His pulses were small volume, barely palpable with cold clammy extremities. A diagnosis of cardiogenic shock secondary to a SVT was made. Intravenous fluid with a plasma expander was administered to correct the shock. He was on nil per oris, continuous positive airway pressure and a urethral catheter to monitor urine output. A cardiologist reviewed and commenced him on oral propranolol initially with slight improvement. He later developed SVT with aberrancy (Figure 1B) for which intravenous amiodarone was given and subsequently changed to oral amiodarone. Vital signs were monitored and subsequently became normal. Feeds were recommenced via cup and spoon. Repeat electrocardiography showed sinus rhythm as shown in Figure 1C. He was discharged home on oral propranolol. Parents were educated on how to monitor oxygen saturation and vital signs at home. He had several episodes of SVT following febrile illnesses after the first episode of arrhythmia. He was recommenced on oral amiodarone, digoxin and propranolol. Their parents were counselled on the management of fever and he was weaned off amiodarone. He is currently being followed up and on low-dose propranolol and digoxin. The last episode of SVT was about 3 months ago. Growth and development have been normal. He is currently 2 years of age. Case 5A 14-month-old female presented with excessive crying of a day duration associated with refusal to feed. There was no history of fever, convulsion or vomiting. She was not on any medication. There was no past history of hospital admissions. On examination, she was conscious, and not irritable. Her anterior fontanelle was patent and normotensive. She was mildly dyspnoeic. The heart rate was 200 bpm and only the first and second heart sounds were heard. An urgent electrocardiograph revealed SVT, echocardiography showed a structurally normal heart. A diagnosis of SVT to rule out Wolff–Parkinson–White syndrome was made. There was no response to vagal manoeuvre. She was commenced on oral propranolol. A repeat electrocardiograph showed a sinus rhythm with a delta wave suggesting Wolff–Parkinson–White syndrome. She has been on follow up and has not had any form of arrhythmia after the first episode. However, she still had delta waves in the last ECG but has been stable on follow up for more than a year. Case 6A 9-year-old male was referred from a general hospital with a 6-year history of recurrent cough, easy fatigability and chest pain. There was associated difficulty in breathing on exertion and palpitation. There was no history of cyanosis, or preceding sore throat before onset of symptoms. He was born at term. He had no developmental delay. He was the first of three children in a monogamous family setting. There were no similar symptoms in his siblings. On examination, he was conscious, tachypnoeic with a hyperactive precordium, a thrill and displaced apex beat. He had grade 4/6 pansystolic murmur loudest at the apex and radiating to the axilla, with gallop rhythm. He also had a tender hepatomegaly. The electrocardiograph revealed atrial flutter. Echocardiography showed aneurysmal dilation of the atrium, prolapse of the anterior mitral valve, thickened mitral valve leaflets, dilated left ventricle, thickened aortic valve leaflet, moderate mitral regurgitation and mild pulmonary hypertension. Antistreptolysin O titre was 87 IU/ml, C-reactive protein was 1.6 mg/l and erythrocyte sedimentation rate was 10 mm/hour. He was admitted and managed for congestive cardiac failure and atrial flutter secondary to rheumatic heart disease. He was commenced on intravenous furosemide initially which was changed to tablet, enalapril, propranolol, digoxin, aspirin and intramuscular benzathine penicillin. His parents were counselled on the need for an urgent surgical intervention. However, he succumbed to the illness while awaiting surgical intervention after about a year of clinic follow up.
Figure 1. (A) SVT in Case 4. (B) SVT with aberrancy and (C) sinus rhythm in the 3-month-old child after the first episode of SVT. Case 7A 10-year-old girl presented with a weak history of cough associated with palpitation. She had a previous history of breathlessness, syncopal attacks and palpitations following febrile illnesses and cough. On examination, she was conscious but dyspnoeic and tachypnoeic with basal crepitation at the left lower zone. A cardiovascular examination revealed a pulse rate of 186 bpm which was regular with no murmur but had a heart rate of 226 bpm. A diagnosis of possible arrhythmia secondary to a respiratory tract infection was considered. An electrocardiograph confirmed SVT. Echocardiography suggested a tachycardia-induced cardiomyopathy, possibly secondary to intermittent SVT was made. A Holter monitoring echocardiograph was requested but was not done due to financial constraints. She was commenced on digoxin tabs, furosemide, enalapril and calcium. A repeat electrocardiography done 48 hours later showed a normal sinus rhythm while an echocardiography done 72 hours later showed a structurally normal heart with good cardiac function. The patient was weaned off the antifailure drugs and discharged. The patient has been on follow up, the fast heartbeat resolved and a repeat electrocardiograph showed sinus rhythm. Case 8A 12-year male, presented with a history of palpitation, syncopal attacks and shortness of breath on moderate exertion of 2 months duration. There was no history of orthopnoea, paroxysmal nocturnal dyspnoea or leg swelling. There was no previous history of hospital admission. There was a similar history in the father who had a pacemaker insertion done in England at 32 years of age. On examination, he was conscious, not dyspnoeic. His pulse was regular, full volume with a rate of 48 bpm. The precordium was active, the heart rate was 50 bpm and the apex beat was at the fifth left intercostal space midclavicular line. Only the first and second heart sounds were heard and there was no murmur. The electrocardiograph showed sinus bradycardia. Echocardiography showed a structurally normal heart. A diagnosis of possible symptomatic familial sinus bradycardia was made but to exclude a complete heart block. His parents were counselled to do a Holter monitoring electrocardiograph which confirmed a sinus bradycardia. The child was referred, at his parents’ request, to a cardiologist in England for further evaluation and intervention. A diagnosis of heart block was confirmed and he was to have a pacemaker insertion. He has been lost to follow up. DISCUSSIONWe retrospectively report the clinical presentation, management and short-term clinical outcomes of eight children, spanning neonatal to adolescent age groups, with different forms of arrhythmias, highlighting challenges experienced in their management. As summarised in Table 1, the forms of arrhythmias included sinus bradycardia, heart block, SVT and atrial flutter. Arrhythmia in children has been documented in both genders. Five of the eight children in our reports were females, this is similar to the report of Clausen et al. [4] and Sadoh et al. [12] who, respectively, reported that 56% and 59% of their subjects were females. The reason for this sex predilection is not immediately clear. Fever, fast breathing and cough were the commonest presenting features in the current report. This is similar to the report of Chockalingam et al. [15] in Chennai. It will, therefore, be appropriate to encourage healthcare practitioners involved in the care of children to always watch out for the possibility of rhythm disorders in children presenting with the above symptoms to encourage early diagnosis and prompt management of rhythm disorders in such children. Arrhythmias in children can present in various forms depending on the underlying aetiology [15]. In this case series, the major form of arrhythmia observed in the neonatal age group was heart block which was mostly due to complex congenital heart defects inclusive of defects of the atrium which may be due to disruption of conduction pathways. Congenital heart block has been associated with atrioventricular septal defect [16]. Detection of foetal bradycardia in utero suggested a rhythm problem in these patients informing the need for a foetal echocardiography which, however, was not done in any of the patients. The immediate reason for this omission is not known; however, it is plausible to assume that it was due to poor awareness on the part of the health practitioner who supervised the antenatal care. Hence, there may be a need to ensure screening of high-risk pregnant women with foetal echocardiography, for example, when findings of obstetric ultrasound are suspicious [17]. Foetal echocardiography can diagnose most significant congenital heart lesions as early as 17–19 weeks of gestation. Also, M-mode echocardiography can diagnose rhythm disturbances in the foetus and give information on the success of antiarrhythmic therapy administered to the mother [18]. Arrhythmias are common in children with CHD [19]. It is either due to coexisting congenital abnormalities of the specialised conduction system or in response to haemodynamic influences on chamber dimensions, muscle mass and metabolism of myocardial tissue [20]. In the current report, all the neonates with arrhythmia had CHD. Rhythm abnormalities in foetuses and neonates may heighten paediatric and obstetrics clinicians’ suspicion of an underlying CHD. Delays in the diagnosis and management of these arrhythmias in these children can contribute to mortality and worsen morbidity in them [19]. SVT is the most common arrhythmia in children as was observed in our report. Venugopalan et al. [8] reported three cases of SVT, each with varying presentations. However, none of the patients reported by Venugopalan et al. [8] presented in infancy and only one had an underlying congenital heart defect. In our case series, none of the three patients with SVT had a CHD. In a prospective study of the prevalence, management and outcome of patients with SVT by Sadoh et al. [12], the age range of the subjects was between 4 months and 6 years [14]. The subjects had varying underlying precipitants of SVT including myocarditis, diarrhoea disease, neuroblastoma, intussusception and caffeine ingestion. None of the subjects had underlying congenital heart defects; however, 4 out of the 29 cases had no identifiable underlying aetiology. The patient who presented in infancy initially had a SVT with aberrant conduction that looked like a ventricular tachycardia which was precipitated by a febrile illness (Table 1). The patient responded to medications but developed two other episodes of SVT with febrile illness which also resolved with medications. Older children with SVT may present with palpitation which was the presentation in one of the patients. SVT has been reported to be exacerbated by exposure to decongestants and bronchodilators. None of the patients in the current series were reported to have taken any of these medications. Wolff–Parkinson–White syndrome was diagnosed in one of the patients. Its typical feature of short P–R interval and delta wave seen when the patient is tachycardia-free was found in this patient. The medications used in these patients with SVT include amiodarone, propranolol and digoxin. The patients did not respond to vagal manoeuvres and adenosine was not readily available. One of the patients developed SVT with febrile illness. Atrial flutter was found in the patient with rheumatic heart disease. It is associated with mitral insufficiency, dilated or large stretched left atrium [1] which was found on echocardiography for this patient. The patient was treated with oral medications including propranolol. The flutter waves improved for a while after serial electrocardiographs; however, later became evident again because parents were unable to afford surgical intervention [15]. Sinus bradycardia results from slow discharge of impulses from the sinus node which is the heart’s natural pacemaker [1]. It is usually without significance, symptomatic familial bradycardia was reported by Laish-Farkash et al. [20] in three unrelated Morrocan Jews. There is also a family history in the patient who had symptomatic bradycardia, although a genetic analysis has not been carried out in this patient [15]. In investigating the patients in the above report, none of the patients had Holter monitoring due to financial constraints. It would have been desirable to have genetic studies done also but this facility is currently not readily available in the country as the samples must be shipped outside the country. This would have helped to rule out genetic causes of rhythm disorders, especially in Case 4 as mentioned above. The treatment of arrhythmias when the underlying cause is well recognised may be challenging. The drug therapies used included propranolol, digoxin and amiodarone. Some of the patients required a pacemaker insertion but only one of them was able to access this therapy outside Nigeria. Perhaps, this highlights the nonavailability of paediatric pacemaker insertion services in Lagos and, by extension, Nigeria, compared to the adult population [22,23]. Adenosine and synchronised cardioversion are recommended modes of treatment in patients with SVT [24]. In the current report, none of the patients with SVT received adenosine or synchronised cardioversion even though there was no response to vagal stimulation. This is because the facilities for the above were not available in the managing centres. This further calls attention to the fact that there are a lot of challenges in the treatment of children with rhythm disorders in Lagos [16]. In terms of the outcome of the patients in this report, three out of the eight patients reported died. This is similar to the report of Sadoh et al. [12]. Two of the cases reported have been lost to follow up while only three are still alive and doing well on follow up. The mortality rate for children with arrhythmia in Lagos, and Nigeria is very high compared with what is obtainable in the developed countries [2]. The current report has not only brought out the need for collaboration with established centres abroad for skill sharing but has also called attention to the urgent need for man-power training and availability of necessary equipment for pacemaker insertion services for Nigerian children so as to be able to salvage children who need this treatment. There is also a need to advocate for further training in surgical procedures especially for complex CHDs. Furthermore, the patient with atrial flutter from rheumatic heart disease was unable to raise funds until he succumbed. In conclusion, arrhythmias can occur in children of different age groups and should be promptly recognised to reduce morbidity and mortality. In our setting, resource constraints pose a significant challenge to the optimal management of children with arrhythmias. Being a retrospective review of a few cases seen in two private practices in Lagos, Nigeria, our report may not accurately represent the true epidemiology and outcomes of paediatric arrhythmias in Lagos or Nigeria. Hence, it will be desirable to have a prospective multicentered study across the country which will provide more information on arrhythmias in Nigeria. ACKNOWLEDGEMENTThe authors gratefully acknowledge patients reported in this clinical review, their parents and other healthcare workers who participated in their care. CONFLICT OF INTERESTThe authors declare that they have no conflicts of interest. FUNDINGNone. CONSENT TO PARTICIPATEWritten informed consent was obtained from parents of children included in the study. ETHICAL APPROVALEthics committee approval was received for this study. REFERENCES
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| How to Cite this Article |
| Pubmed Style Animasahun BA, Oladimeji AB, Lamina MO, Solarin AU, Disu EA. Rhythm abnormalities among hospitalized children in Lagos: A case series. Sudan J Paed. 2023; 23(2): 224-233. doi:10.24911/SJP.106-1564007487 Web Style Animasahun BA, Oladimeji AB, Lamina MO, Solarin AU, Disu EA. Rhythm abnormalities among hospitalized children in Lagos: A case series. https://sudanjp.com//?mno=58413 [Access: February 05, 2026]. doi:10.24911/SJP.106-1564007487 AMA (American Medical Association) Style Animasahun BA, Oladimeji AB, Lamina MO, Solarin AU, Disu EA. Rhythm abnormalities among hospitalized children in Lagos: A case series. Sudan J Paed. 2023; 23(2): 224-233. doi:10.24911/SJP.106-1564007487 Vancouver/ICMJE Style Animasahun BA, Oladimeji AB, Lamina MO, Solarin AU, Disu EA. Rhythm abnormalities among hospitalized children in Lagos: A case series. Sudan J Paed. (2023), [cited February 05, 2026]; 23(2): 224-233. doi:10.24911/SJP.106-1564007487 Harvard Style Animasahun, B. A., Oladimeji, . A. B., Lamina, . M. O., Solarin, . A. U. & Disu, . E. A. (2023) Rhythm abnormalities among hospitalized children in Lagos: A case series. Sudan J Paed, 23 (2), 224-233. doi:10.24911/SJP.106-1564007487 Turabian Style Animasahun, Barakat A., Alaba B. Oladimeji, Moriam O. Lamina, Adaobi U. Solarin, and Elizabeth A. Disu. 2023. Rhythm abnormalities among hospitalized children in Lagos: A case series. Sudanese Journal of Paediatrics, 23 (2), 224-233. doi:10.24911/SJP.106-1564007487 Chicago Style Animasahun, Barakat A., Alaba B. Oladimeji, Moriam O. Lamina, Adaobi U. Solarin, and Elizabeth A. Disu. "Rhythm abnormalities among hospitalized children in Lagos: A case series." Sudanese Journal of Paediatrics 23 (2023), 224-233. doi:10.24911/SJP.106-1564007487 MLA (The Modern Language Association) Style Animasahun, Barakat A., Alaba B. Oladimeji, Moriam O. Lamina, Adaobi U. Solarin, and Elizabeth A. Disu. "Rhythm abnormalities among hospitalized children in Lagos: A case series." Sudanese Journal of Paediatrics 23.2 (2023), 224-233. Print. doi:10.24911/SJP.106-1564007487 APA (American Psychological Association) Style Animasahun, B. A., Oladimeji, . A. B., Lamina, . M. O., Solarin, . A. U. & Disu, . E. A. (2023) Rhythm abnormalities among hospitalized children in Lagos: A case series. Sudanese Journal of Paediatrics, 23 (2), 224-233. doi:10.24911/SJP.106-1564007487 |
Nagwa Salih, Ishag Eisa, Daresalam Ishag, Intisar Ibrahim, Sulafa Ali
Sudan J Paed. 2018; 18(1): 24-27
» Abstract » doi: 10.24911/SJP.2018.1.4
Siba Prosad Paul, Emily Natasha Kirkham, Katherine Amy Hawton, Paul Anthony Mannix
Sudan J Paed. 2018; 18(2): 5-14
» Abstract » doi: 10.24911/SJP.106-1519511375
Inaam Noureldyme Mohammed, Soad Abdalaziz Suliman, Maha A Elseed, Ahlam Abdalrhman Hamed, Mohamed Osman Babiker, Shaimaa Osman Taha
Sudan J Paed. 2018; 18(1): 48-56
» Abstract » doi: 10.24911/SJP.2018.1.7
Adnan Mahmmood Usmani; Sultan Ayoub Meo
Sudan J Paed. 2011; 11(1): 6-7
» Abstract
Mustafa Abdalla M. Salih, Mohammed Osman Swar
Sudan J Paed. 2018; 18(1): 2-5
» Abstract » doi: 10.24911/SJP.2018.1.1
Amir Babiker, Afnan Alawi, Mohsen Al Atawi, Ibrahim Al Alwan
Sudan J Paed. 2020; 20(1): 13-19
» Abstract » doi: 10.24911/SJP.106-1587138942
Bashir Abdrhman Bashir, Suhair Abdrahim Othman
Sudan J Paed. 2019; 19(2): 81-83
» Abstract » doi: 10.24911/SJP.106-1566075225
Anita Mehta, Arvind Kumar Rathi, Komal Prasad Kushwaha, Abhishek Singh
Sudan J Paed. 2018; 18(1): 39-47
» Abstract » doi: 10.24911/SJP.2018.1.6
Majid Alfadhel, Amir Babiker
Sudan J Paed. 2018; 18(1): 10-23
» Abstract » doi: 10.24911/SJP.2018.1.3
Amir Babiker, Mohammed Al Dubayee
Sudan J Paed. 2017; 17(2): 11-20
» Abstract » doi: 10.24911/SJP.2017.2.12